| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Original Article
Volume 13, Number 3, August 2023, pages 104-113
Prevalence of Metabolically-Obese Normal-Weight Worldwide: Systematic Review and Meta-Analysis
Gianella Zulema Zenas-Trujilloa, e , Irma Trujillo-Ramirezb
, Jesus Maritza Carhuavilca-Torresc
, Ronald Espiritu Ayala-Mendivilb
, Victor Juan Vera-Poncea, d
aInstituto de Investigacion en Ciencias Biomedicas, Universidad Ricardo Palma, Lima, Peru
bUnidad de Posgrado, Facultad de Medicina, Universidad Nacional Mayor San Marcos, Lima, Peru
cUniversidad Cientifica del Sur, Lima, Peru
dUniversidad Tecnologica del Peru, Lima, Peru
eCorresponding Author: Gianella Zulema Zenas-Trujillo, Instituto de Investigacion en Ciencias Biomedicas, Universidad Ricardo Palma, Lima, Peru
Manuscript submitted May 7, 2023, accepted June 17, 2023, published online July 12, 2023
Short title: Prevalence of MONW Worldwide
doi: https://doi.org/10.14740/jem882
| Abstract | ▴Top |
Background: Obesity causes the loss of body homeostasis and predisposes to the development of disease; some individuals present alterations described even having a normal body mass index (BMI), and these are called thin metabolically obese. The objective was to carry out a systematic review with meta-analysis to determine the prevalence of metabolically-obese normal-weight (MONW) worldwide.
Methods: The search for studies was conducted from May to June 2022 in the EMBASE, PubMed, WOS, and Scopus databases. The purification and ordering of data were carried out using the Excel 2016 program, later a meta-analysis with the Stata version 17 program.
Results: A total of 408,251 people with normal BMI were identified, of whom 78,054 had a metabolic disorder, and the prevalence after the meta-analysis was 26.78% (95% confidence interval: 18.45 - 36.03) with high heterogeneity (I2 = 99.86%).
Conclusion: The findings of the systematic review confirm a high prevalence of MONW worldwide.
Keywords: Systematic review; Metabolically-obese normal-weight; Obesity; Prevalence
| Introduction | ▴Top |
The prevalence of obesity has doubled in the last four decades in more than 70 countries [1]. According to the World Health Organization (WHO), in 2016, 650 million adults worldwide were obese [2]. While in Latin America, it is estimated that about 58% of the region’s inhabitants live with overweight [3]. In Peru, according to a report prepared at the national level, the prevalence of obesity increased by 6.3%, since it went from 18.3% in 2013 to 24.6% in 2020 [4].
Obesity causes loss of body homeostasis and predisposes to developing some diseases such as type 2 diabetes mellitus, hypertension, liver disease, cancer, allergies, osteoporosis and sarcopenia [5]. Nevertheless, despite the relationship between obesity and its comorbidities, some individuals present alterations described even having a body mass index (BMI) within normal values, and these are called metabolically-obese normal-weigh (MONW) [6].
Due to the absence of excess body weight, MONW people easily mask their condition, creating the need for screening and consequently delaying diagnosis and treatment [7]. The prevalence of MONW in adults has inadvertently increased over the years. Taking a study carried out in Iran in 1996 [8] as an example, the prevalence was 16.06%, but 20 years later, another study conducted in the same country found a prevalence of 34.82%.
Currently, it is estimated that the prevalence of MONW is approximately 30.04% worldwide [9]; however, up to the time of this review, no study was found that scrupulously classified the samples of the included manuscripts. Therefore, due to the challenge it represents to public health and all of those mentioned above, the objective of this article was to carry out a systematic review with meta-analysis of the prevalence of MONW worldwide.
| Materials and Methods | ▴Top |
Study design
This study was a systematic review with meta-analysis that synthesizes the current information on the prevalence of MONW worldwide. For this, the manuscript was carried out following the PRISMA method.
Definition of MONW
Metabolically healthy people are those without metabolic alterations and any associated disease, although the definition varies according to the author [10]. Likewise, the WHO defines a person of normal weight as those with a BMI of 18.5 to 24.9. Therefore, for this review, we considered MONW in subjects with a normal BMI, but with metabolic alterations.
Selection criteria
Studies were included that 1) had a probability sample; 2) included the total number of MONW of patients with normal BMI; 3) participants were ≥ 18 years of age; 4) cross-sectional studies; 5) if they used a criterion to define the MONW patient; 6) if they used the BMI as a criterion to define whether the patient was obese. We excluded 1) systematic reviews and letters to the editor; 2) studies whose total population had a BMI above or below the normal range; 3) studies whose participants had a prior diagnosis of any communicable or non-communicable disease.
Search strategy
The search for studies was carried out from May to June 2022 in the EMBASE, PubMed, WOS, and Scopus databases. The search formula can be found in Supplementary Material 1 (www.jofem.org). No distinction was made regarding the language or the date on which the studies were prepared. Additionally, references of the included studies were checked for additional relevant articles.
Synthesis and analysis
Data filtering and ordering was carried out using the Excel 2016 program, and later a meta-analysis for prevalence was carried out with the program Stata version 17. Two analyses were done, one with all studies and then only with those that met the criteria according to the Newcastle-Ottawa Scale [11] for a truly representative sample.
Ethical compliance with human
The article was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Selection of studies
After the search was carried out, duplicates were removed. The results were downloaded. Two authors (VJVP and ITR) screened the title and abstract of each manuscript, selecting those consistent with the review theme, and then two researchers (ITR and GZZT) reviewed the full texts in order to define whether the manuscripts complied, in effect, with the selection criteria. In the case of any discrepancy, it was resolved by a third researcher (VJVP). For both stages, the Rayyan online software was used (Fig. 1).
 Click for large image | Figure 1. Flow chart. |
Extraction of information
For the extraction of information, a file created by the authors was elaborated (Table 1). The data extraction was carried out by JALC and GZZT to be later verified by VJVP in order to verify their accuracy.
 Click to view | Table 1. Criteria Used to Define Metabolic Disorders |
Risk of bias
An adaptation of the Newcastle-Ottawa Scale for descriptive cross-sectional studies was used (Supplementary Material 2, www.jofem.org). The evaluation was done in duplicate to avoid any bias. Finally, only those manuscripts with a representative or random sample of the population (classification A or B, according to the Newcastle-Ottawa Scale) were selected [11].
The most used criteria to diagnose MONW in the studies included in this review are summarized in Table 1.
| Results | ▴Top |
Study characteristics
Of the 920 manuscripts identified, 26 were selected (Fig. 1). The oldest study was published in 1987, while the most current ones were carried out in 2018. It was found that 23 studies used one of these three criteria: the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III), the International Diabetes Federation (IDF), and the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) or Joint Interim Statement (JIS) (Table 1); while three manuscripts used others (Supplementary Material 2, www.jofem.org). The characteristics of the included studies are shown in Table 2 [8, 9, 12-35].
 Click to view | Table 2. Characteristics of the Studies Included in the Review |
A total of 408,251 people with normal BMI were identified, of which 78,054 had a metabolic disorder, therefore the prevalence of MONW worldwide according to the present review would be 19.11%.
The data were collected from 26 studies; 26.92% of the studies were conducted in China (n = 7) [9, 17, 20, 21, 23, 28, 33], 19.23% (n = 5) [8, 15, 29-31] in Iran, and 11.53% (n = 3) [13, 16, 25] in Korea. In addition, it was reviewed three countries with the same number of studies (n = 2), representing 7.69% each: United States [12, 19], Spain [14, 18], and Poland [22, 35]; finally another five countries [24, 26, 27, 32, 34] (Peru, Italy, The Netherlands, Iceland and Palestine) represented 15.36% of the total manuscripts (3.84% each, n = 1) (Fig. 2). In Asia, the total MONW sample represented 80.65% (n = 62,954) of cases worldwide; in America, it was 3.99% (n = 3,120), and in Europe 5.34% (n = 11,980).
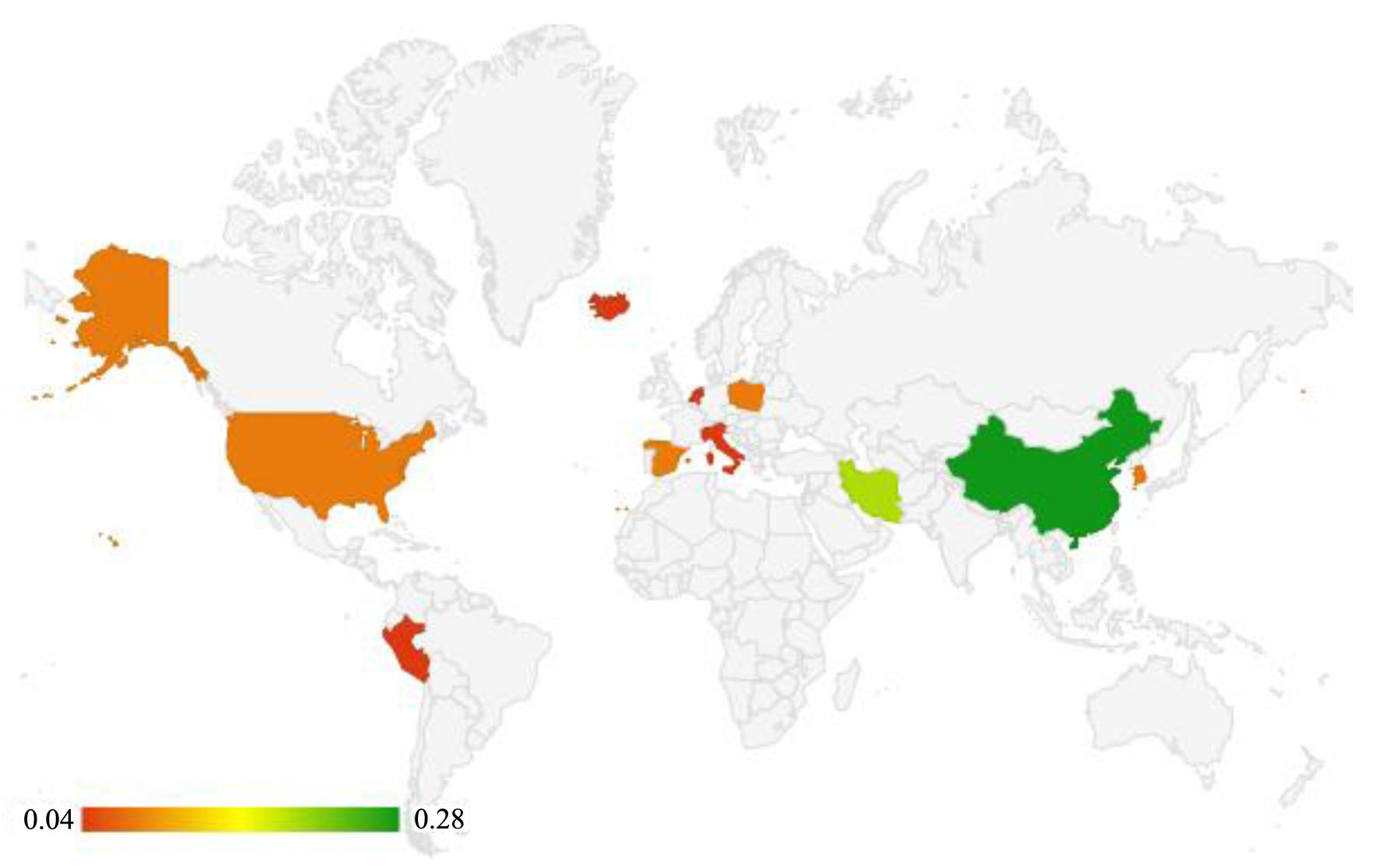 Click for large image | Figure 2. Regional prevalence of the studies selected for the review. |
Finally, the prevalence of MONW recorded each year has been increasing progressively, going from 9.18% in 1987 to 52.46% in 2012.
Meta-analysis
Of the studies included in the systematic review, those with a truly representative sample according to the New Castle-Ottawa Scale (all subjects or random sampling) were selected for meta-analysis. The study carried out by Suliga et al [22] was the one with the highest prevalence with 47.20% (95% confidence interval (CI): 46.35 - 48.05), while the manuscript by Hadaegh et al [15] had the lowest prevalence with 10.48% (95% CI: 9.50 - 11.55). Thus, the joint prevalence was 26.78% (95% CI: 18.45 - 36.03); however, it should be noted that there was high heterogeneity (I2 = 99.86%) (Fig. 3).
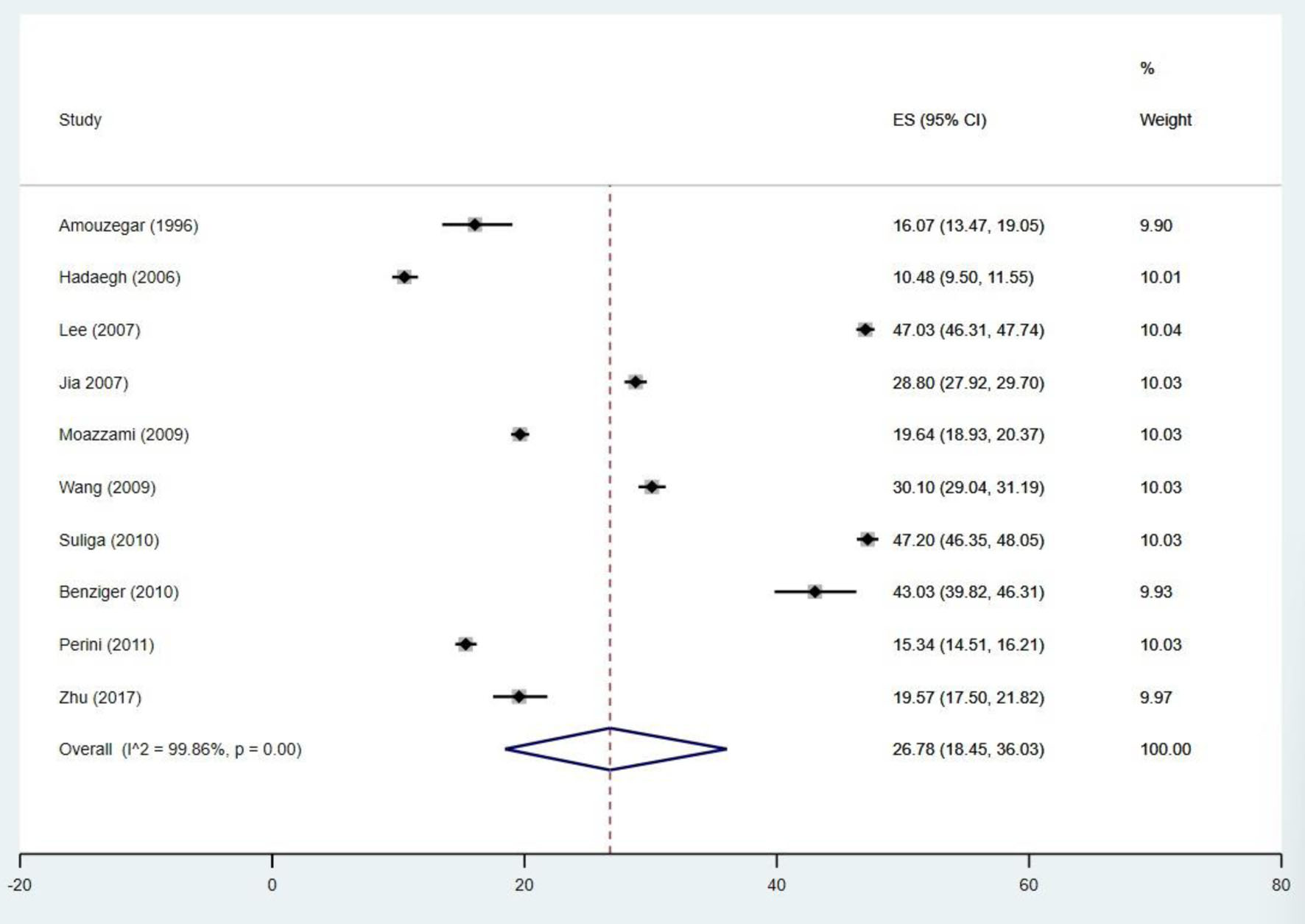 Click for large image | Figure 3. Forest plot of the prevalence of studies with truly representative samples. |
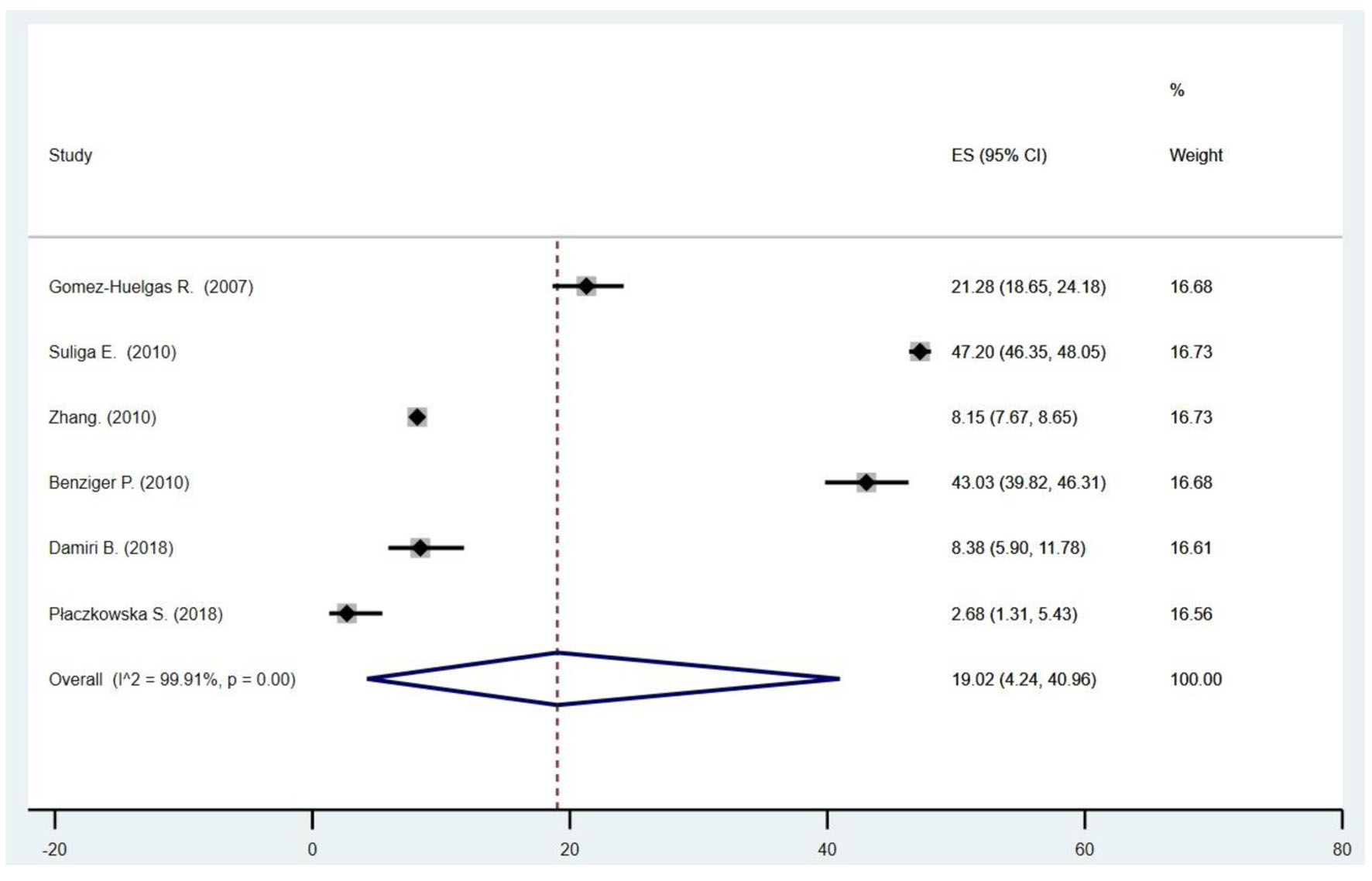
In order to prove if heterogeneity may have been secondary to the different criteria used for metabolic disorder, meta-analyses were performed between studies that used the same criteria (Figs. 4-7).
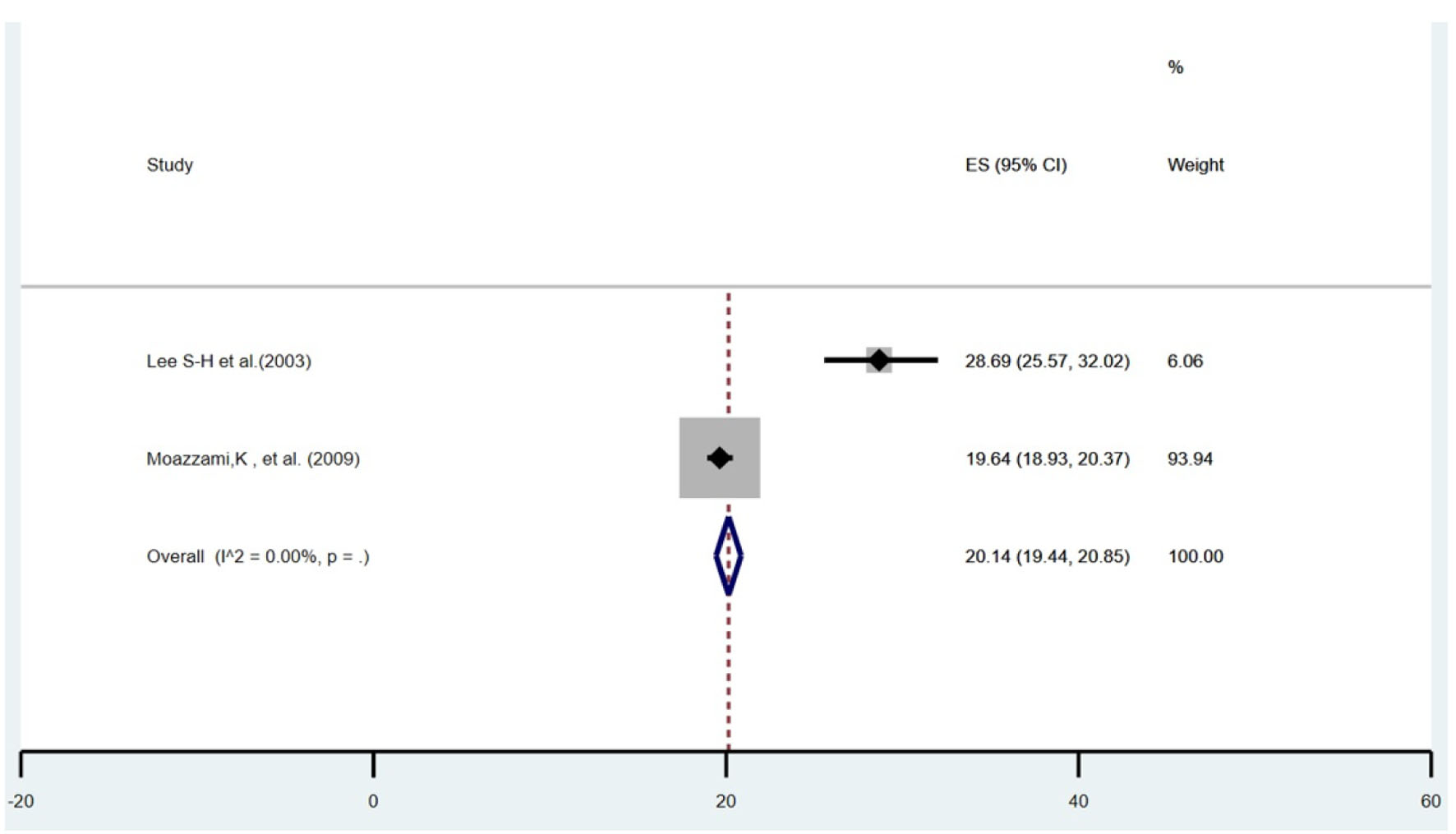 Click for large image | Figure 4. Forest plot of the studies that consider the AHA/NHLBI criteria for the diagnosis of metabolic disorder. |
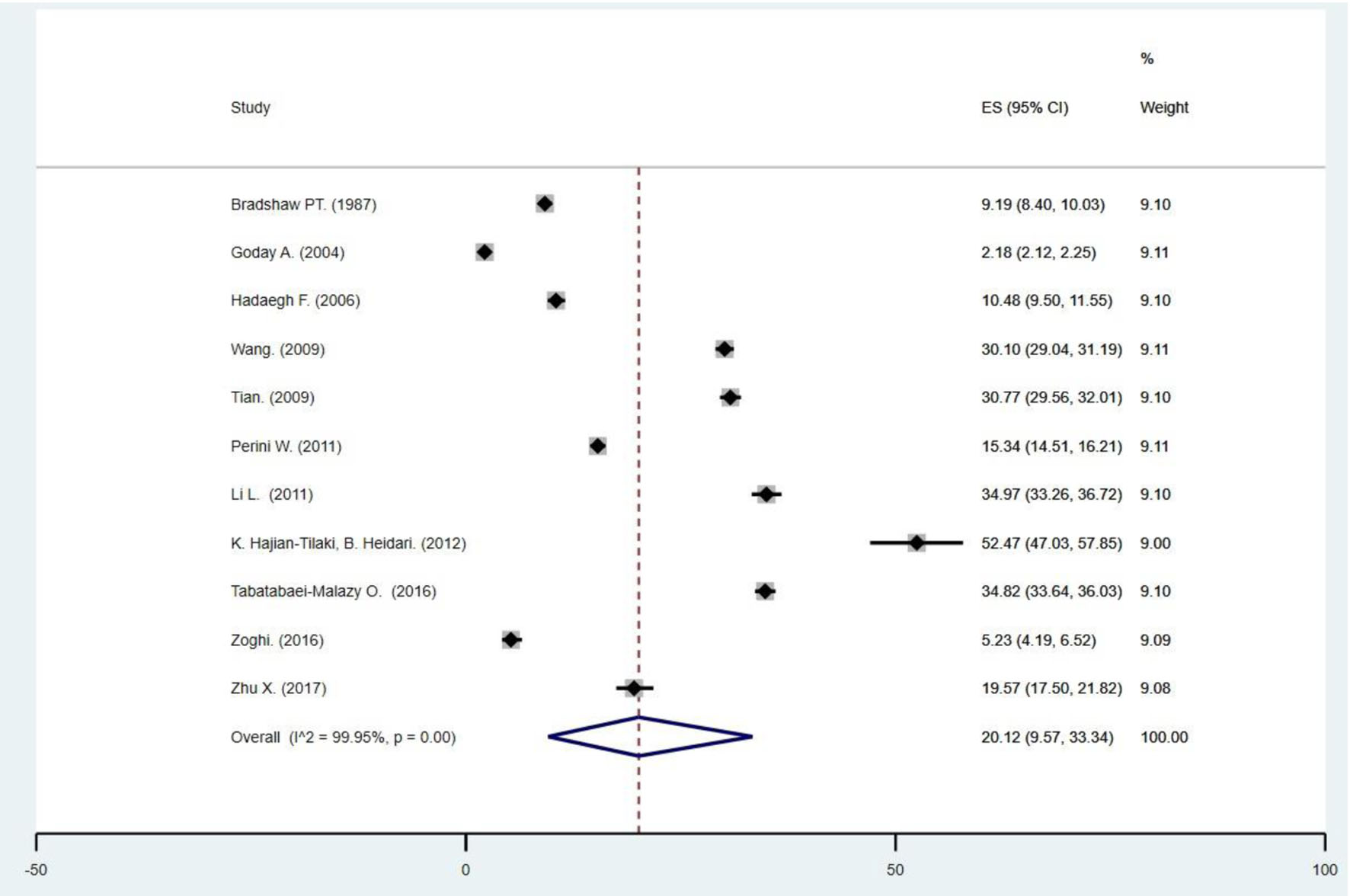 Click for large image | Figure 5. Forest plot of the studies that consider ATP III criteria for the diagnosis of metabolic disorder. |
 Click for large image | Figure 6. Forest plot of the studies that consider IDF criteria for the diagnosis of metabolic disorder. |
 Click for large image | Figure 7. Forest plot of the studies that consider JIS criteria for the diagnosis of metabolic disorder. |
Despite the forest plots carried out, we still point out a high heterogeneity, with the exception of the studies that used the AHA/NHLBI as criteria (Fig. 4).
| Discussion | ▴Top |
In this article, the prevalence of MONW in people with normal BMI has been reviewed. Of the 26 selected studies, only 38.46% (n = 10) were considered for the meta-analysis.
The present review addressed the prevalence of MONW in the adult population worldwide. The overall prevalence and post-meta-analysis prevalence were 21.92% (95% CI: 12.79 - 32.69) (Supplementary Material 2, www.jofem.org) and 26.78% (95% CI: 18.45 - 36.03), respectively. These results agree with those found in a meta-analysis conducted by Wang et al [9], in which the general prevalence of MONW in people with normal weight was 30.04% (95% CI: 25.59 - 35.57).
However, unlike the previously mentioned article, in which populations of European origin had the highest prevalences [9], in this study, a higher prevalence of MONW people was found in Asian populations. There is evidence [36] that Asian populations are less obese, but with greater susceptibility to metabolic disorders compared to Caucasians. This could be because they have higher visceral adipose tissue with similar levels of obesity.
There are some limitations that should be considered in our review. An important limitation of this review is that the sample was only collected from 11 countries, which limits the generalization to the worldwide prevalence. Furthermore, most of the Asian studies were conducted in China, only three were conducted in South Korea, and none were conducted in Japan, so they were not representative of the entire Asian population. In addition, it is important to point out that in this study, factors that influence the development of a metabolically unhealthy phenotype in subjects with normal weight were not considered [37] such as physical activity, genetics, lifestyle, tobacco and alcohol consumption; the latter two, according to the meta-analysis prepared by Wang et al, significantly increase the prevalence of MONW since they significantly impair metabolic health [9]. Finally, the heterogeneity between the vast majority of studies that used the same diagnostic criterion (ATP III, IDF, and JIS) reflects that this is mainly due to the relationship between metabolic disorders and lifestyles rather than using different criteria.
Nevertheless, we emphasize the need for a common definition because we found two studies carried out in different countries and years that diagnosed metabolic disorders with the same criterion (AHA/NHLBI) did not have heterogeneity.
Conclusion
This systematic review and meta-analysis confirm a high prevalence of MONW worldwide. Likewise, the need to develop a uniform criterion that can be used by clinical and research groups to diagnose MONW is highlighted.
| Supplementary Material | ▴Top |
Suppl 1. Different terms that were used to search for manuscripts in different databases.
Suppl 2. Studies truly representative and with a justified sample size according to the Newcastle-Ottawa Scale; other criteria used to define metabolic alterations; forest plot of the prevalence of all the studies.
Acknowledgments
None to declare.
Financial Disclosure
This study did not receive any funding in any form.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
GZZT and VJVP participated in the genesis of the idea, project design, development. The authors JMCT, REAM and ITR participated in collection and interpretation of data, analysis of the results and preparation of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Collaborators GBDO, Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13-27.
doi pubmed pmc - Obesity [Internet]. Citado el 23 de enero de 2023. Disponible en: https://www.who.int/health-topics/obesity.
- Mitchell C. https://www.facebook.com/pahowho.OPS/OMS | Sobrepeso afecta a casi la mitad de la poblacion de todos los paises de America Latina y el Caribe salvo por Haití [Internet]. Pan American Health Organization / World Health Organization. 2017 [citado el 23 de enero de 2023]. Disponible en: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=12911:overweight-affects-half-population-latin-americacaribbean-except-haiti&Itemid=0&lang=es#gsc.tab=0.
- INEI - Peru: Enfermedades No Transmisibles y Transmisibles, 2020 [Internet]. [citado el 31 de enero de 2023]. Disponible en: https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1796/.
- Barakat B, Almeida MEF. Biochemical and immunological changes in obesity. Arch Biochem Biophys. 2021;708:108951.
doi pubmed - Pluta W, Dudzinska W, Lubkowska A. Metabolic obesity in people with normal body weight (MONW)-review of diagnostic criteria. Int J Environ Res Public Health. 2022;19(2):624.
doi pubmed pmc - Pastusiak K, Przysławski J. The criteria of the identification of metabolic obesity among people with normal body weight and their use in everyday practice. Journal of Medical Science. 2018;87(1):34-39.
doi - Amouzegar A, Kazemian E, Abdi H, Mansournia MA, Bakhtiyari M, Hosseini MS, Azizi F. Association between thyroid function and development of different obesity phenotypes in euthyroid adults: a nine-year follow-up. Thyroid. 2018;28(4):458-464.
doi pubmed - Wang B, Zhuang R, Luo X, Yin L, Pang C, Feng T, You H, et al. Prevalence of metabolically healthy obese and metabolically obese but normal weight in adults worldwide: a meta-analysis. Horm Metab Res. 2015;47(11):839-845.
doi pubmed - Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011;9:48.
doi pubmed pmc - Ottawa Hospital Research Institute [Internet]. [citado el 4 de febrero de 2023]. Disponible en: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- Bradshaw PT, Monda KL, Stevens J. Metabolic syndrome in healthy obese, overweight, and normal weight individuals: the Atherosclerosis Risk in Communities Study. Obesity (Silver Spring). 2013;21(1):203-209.
doi pubmed pmc - Lee SH, Ha HS, Park YJ, Lee JH, Yim HW, Yoon KH, Kang MI, et al. Identifying metabolically obese but normal-weight (MONW) individuals in a nondiabetic Korean population: the Chungju Metabolic disease Cohort (CMC) study. Clin Endocrinol (Oxf). 2011;75(4):475-481.
doi pubmed - Goday A, Calvo E, Vazquez LA, Caveda E, Margallo T, Catalina-Romero C, Reviriego J. Prevalence and clinical characteristics of metabolically healthy obese individuals and other obese/non-obese metabolic phenotypes in a working population: results from the Icaria study. BMC Public Health. 2016;16:248.
doi pubmed pmc - Hadaegh F, Zabetian A, Harati H, Azizi F. Metabolic syndrome in normal-weight Iranian adults. Ann Saudi Med. 2007;27(1):18-24.
doi pubmed pmc - Lee J, Kwak SY, Park D, Kim GE, Park CY, Shin MJ. Prolonged or transition to metabolically unhealthy status, regardless of obesity status, is associated with higher risk of cardiovascular disease incidence and mortality in Koreans. Nutrients. 2022;14(8):1644.
doi pubmed pmc - Jia A, Xu S, Xing Y, Zhang W, Yu X, Zhao Y, Ming J, et al. Prevalence and cardiometabolic risks of normal weight obesity in Chinese population: A nationwide study. Nutr Metab Cardiovasc Dis. 2018;28(10):1045-1053.
doi pubmed - Gomez-Huelgas R, Narankiewicz D, Villalobos A, Warnberg J, Mancera-Romero J, Cuesta AL, Tinahones FJ, et al. Prevalence of metabolically discordant phenotypes in a mediterranean population-The IMAP study. Endocr Pract. 2013;19(5):758-768.
doi pubmed - Moazzami K, Lima BB, Sullivan S, Shah A, Bremner JD, Vaccarino V. Independent and joint association of obesity and metabolic syndrome with depression and inflammation. Health Psychol. 2019;38(7):586-595.
doi pubmed pmc - Tian S, Xu Y, Dong H. The effect of metabolic health and obesity phenotypes on risk of hypertension: A nationwide population-based study using 5 representative definitions of metabolic health. Medicine (Baltimore). 2018;97(38):e12425.
doi pubmed pmc - Zheng Q, Lin W, Liu C, Zhou Y, Chen T, Zhang L, Zhang X, et al. Prevalence and epidemiological determinants of metabolically obese but normal-weight in Chinese population. BMC Public Health. 2020;20(1):487.
doi pubmed pmc - Suliga E, Koziel D, Gluszek S. Prevalence of metabolic syndrome in normal weight individuals. Ann Agric Environ Med. 2016;23(4):631-635.
doi pubmed - Zhang Y, Fu J, Yang S, Yang M, Liu A, Wang L, Cao S, et al. Prevalence of metabolically obese but normal weight (MONW) and metabolically healthy but obese (MHO) in Chinese Beijing urban subjects. Biosci Trends. 2017;11(4):418-426.
doi pubmed - Benziger CP, Bernabe-Ortiz A, Gilman RH, Checkley W, Smeeth L, Malaga G, Miranda JJ, et al. Metabolic abnormalities are common among south american hispanics subjects with normal weight or excess body weight: the CRONICAS cohort study. PLoS One. 2015;10(11):e0138968.
doi pubmed pmc - Kim MH, Chang Y, Jung HS, Shin H, Ryu S. Impact of self-rated health on progression to a metabolically unhealthy phenotype in metabolically healthy obese and non-obese individuals. J Clin Med. 2019;8(1):34.
doi pubmed pmc - Buscemi S, Chiarello P, Buscemi C, Corleo D, Massenti MF, Barile AM, Rosafio G, et al. Characterization of metabolically healthy obese people and metabolically unhealthy normal-weight people in a general population cohort of the ABCD study. J Diabetes Res. 2017;2017:9294038.
doi pubmed pmc - Perini W, Kunst AE, Snijder MB, Peters RJG, van Valkengoed IGM. Ethnic differences in metabolic cardiovascular risk among normal weight individuals: Implications for cardiovascular risk screening. The HELIUS study. Nutr Metab Cardiovasc Dis. 2019;29(1):15-22.
doi pubmed - Li L, Chen K, Wang AP, Gao JQ, Zhao K, Wang HB, Dou JT, et al. Cardiovascular disease outcomes in metabolically healthy obesity in communities of Beijing cohort study. Int J Clin Pract. 2018;73(3):e13279.
doi pubmed - Hajian-Tilaki K, Heidari B. Metabolically healthy obese and unhealthy normal weight in Iranian adult population: Prevalence and the associated factors. Diabetes Metab Syndr. 2018;12(2):129-134.
doi pubmed - Tabatabaei-Malazy O, Saeedi Moghaddam S, Masinaei M, Rezaei N, Mohammadi Fateh S, Dilmaghani-Marand A, Abdolhamidi E, et al. Association between being metabolically healthy/unhealthy and metabolic syndrome in Iranian adults. PLoS One. 2022;17(1):e0262246.
doi pubmed pmc - Zoghi G, Shahbazi R, Mahmoodi M, Nejatizadeh A, Kheirandish M. Prevalence of metabolically unhealthy obesity, overweight, and normal weight and the associated risk factors in a southern coastal region, Iran (the PERSIAN cohort study): a cross-sectional study. BMC Public Health. 2021;21(1):2011.
doi pubmed pmc - Olafsdottir AS, Torfadottir JE, Arngrimsson SA. Health behavior and metabolic risk factors associated with normal weight obesity in adolescents. PLoS One. 2016;11(8):e0161451.
doi pubmed pmc - Zhu X, Hu J, Guo H, Ji D, Yuan D, Li M, Yan T, et al. Effect of metabolic health and obesity phenotype on risk of diabetes mellitus: a population-based longitudinal study. Diabetes Metab Syndr Obes. 2021;14:3485-3498.
doi pubmed pmc - Damiri B, Badran L, Safadi D, Sawalha A, Yasin Y, Sawalha M, et al. Metabolic syndrome and related risk factors among adults in the northern West Bank, a cross-sectional study. International Health. 2022;14(4):339-345.
doi - Placzkowska S, Pawlik-Sobecka L, Kokot I, Piwowar A. The association between serum uric acid and features of metabolic disturbances in young adults. Arch Med Sci. 2021;17(5):1277-1285.
doi pubmed pmc - T Kadowaki. Japanese men have larger areas of visceral adipose tissue than Caucasian men in the same levels of waist circumference in a population-based study. International Journal of Obesity [Internet]. [citado el 19 de enero de 2023]. Disponible en: https://www.nature.com/articles/0803248.
- Gomez-Zorita. Thieme E-Journals - Hormone and Metabolic Research / Abstract [Internet]. [citado el 19 de enero de 2023]. Disponible en: https://www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0035-1559767.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
