| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Original Article
Volume 14, Number 1, February 2024, pages 13-20
Waist Body Mass Index Outperforms Other Anthropometric Indicators in Identifying Obesity Using Bioimpedance
Victor Juan Vera-Poncea, f , Fiorella E. Zuzunaga-Montoyab
, Joan A. Loayza-Castroa
, Luisa Erika Milagros Vasquez-Romeroa
, Cori Raquel Iturregui Paucarc
, Mario J. Valladares-Garridod, e
, Willy Ramosa
, Norka Rocio Guillen Poncea
, Jhony A. De La Cruz-Vargasa
aInstituto de Investigaciones en Ciencias Biomedicas, Universidad Ricardo Palma, Lima, Peru
bInstituto de Investigacion de Enfermedades Tropicales, Universidad Nacional Toribio Rodriguez de Mendoza de Amazonas (UNTRM), Amazonas, Peru
cFacultad de Psicologia, Universidad Tecnologica del Peru, Lima, Peru
dEscuela de Medicina, Universidad Continental Lima, Peru
eOficina de Epidemiologia, Hospital Regional Lambayeque, Chiclayo, Peru
fCorresponding Author: Victor Juan Vera-Ponce, Instituto de Investigaciones en Ciencias Biomedicas, Universidad Ricardo Palma, Lima, Peru
Manuscript submitted November 27, 2023, accepted January 10, 2024, published online February 29, 2024
Short title: wBMI Identifies Obesity Using Bioimpedance
doi: https://doi.org/10.14740/jem918
| Abstract | ▴Top |
Background: While the body mass index (BMI) has been widely used to diagnose overweight and obesity, other anthropometric markers, such as waist circumference (WC), waist-to-height ratio (WHtR), among others, have been proposed as alternative diagnostic measures for obesity. The objective was to determine which anthropometric marker has the best diagnostic accuracy for obesity.
Methods: This was a diagnostic test study with the primary analysis in workers of an occupational clinic located in Lima, Peru. The percentage of fat measured by bioimpedance was used as the reference test. The WC, BMI, WHtR, tri-ponderal mass index, new BMI, Clinica Universidad de Navarra-Body Adiposity Estimator (CUN-BAE), and waist BMI (wBMI) were evaluated. Receiver operating characteristic (ROC) curve analysis was used as a statistical and graphical method to assess predictive capacity, as well as the area under the curve (AUC) corresponding to each response variable. Sensitivity and specificity, with their 95% confidence intervals (95% CIs), were calculated.
Results: In our study on obesity according to the percentage of fat, 780 participants were included. The overall prevalence of obesity was 19.74%. Regarding the diagnostic test analysis, the measure with the highest accuracy in women was wBMI: AUC = 0.783 (95% CI: 0.735 - 0.830), sensitivity = 71.59% (95% CI: 60.98 - 80.69), and specificity = 74.54% (95% CI: 69.45 - 79.18). For men, the measure with the highest accuracy was wBMI: AUC = 0.828 (95% CI: 0.779 - 0.878), sensitivity = 89.39% (95% CI: 79.36 - 95.62), and specificity = 58% (95% CI: 52.19 - 63.65).
Conclusions: Our study concludes that wBMI proved to be a superior tool for diagnosing obesity compared to conventional measures such as BMI, WC, WHtR, and other evaluated anthropometric metrics.
Keywords: Obesity; Body mass index; Waist circumference; Waist-to-height ratio; Sensitivity and specificity
| Introduction | ▴Top |
Obesity is a worldwide health calamity impacting nearly 20% of the planet’s adult inhabitants [1]. This condition is associated with a variety of chronic health issues, such as cardiovascular disease, type 2 diabetes mellitus (T2DM), and certain types of malignant growth [2, 3]. Due to its effect on wellbeing and the worldwide economy, it has become indispensable to ascertain successful and accurate systems for its early discovery and administration [4].
Usually, the body mass index (BMI) is widely used to analyze overweight and obesity; on the other hand, a number of researches have demonstrated that it fails to differentiate between fat mass and lean mass or seize abdominal fat distribution [5]. Because of this, other anthropometric markers, for example waist circumference (WC), waist-to-height ratio (WHtR), between others, have been proposed as substitute or additional steps of obesity. Yet, it remains unclear if any of those measures have a distinct benefit over BMI for the assessment of obesity, especially in terms of diagnostic precision [6-8].
Given the above, the objective of this study was to determine which anthropometric indicator has the best diagnostic accuracy for obesity.
| Materials and Methods | ▴Top |
Study design and context
A diagnostic test study was conducted with the primary analysis involving workers from an occupational clinic in Lima, Peru, during the period from March 3 to June 5, 2023. The guidelines of the Standards for Reporting Diagnostic Accuracy Studies (STARD) statement were followed in the preparation of this study [9].
Population, sample, and eligibility criteria
The population consisted of workers aged between 18 and 65 years. They belonged to different companies in Lima, Peru, whose main work areas are: administrative, management, accounting, assistant, supervisor, bricklayer, operator, driver, and analyst.
There was no sampling frame. The unit of examination was the employee. The sample contained employees meeting the inclusion standards: 1) having measurements of the body, such as weight, height, and WC; 2) staff presenting for work assessment at the clinic during the study time period; and 3) individuals aged 18 to 65 years. Excluded from the study were pregnant women, as weight gained during pregnancy can confound measurements of obesity; individuals who declined to provide informed consent; persons with known medical conditions impacting body structure such as thyroid diseases or chronic kidney disease; users of medications that may alter body weight or structure for instance corticosteroids, antidepressants, or diabetes drugs; those presently undergoing treatment for being overweight or obese; and participants incapable of undergoing measurements of the body or bioimpedance testing due to any cause including injuries.
The sample selection for the study was carried out using non-probabilistic consecutive sampling. In this case, all adult workers who came to the clinic for their occupational evaluation during the study period and met the inclusion/exclusion criteria were invited to participate.
Sample size
The sample size was calculated using the Epidat program (meaning of the acronym). Referring to the literature, specifically the study by Romero-Corral et al [5] assessing the accuracy of BMI for obesity, an expected sensitivity and specificity of 83% and 76%, respectively, along with an accuracy of 4%, resulted in a calculated sample size of 777 individuals.
Given the expectation of a rejection rate of around 50%, it was planned to evaluate a total of 1,554 workers. However, to ensure reaching this number, and anticipating that only 80% of the workers approached would meet the eligibility criteria for the study, it was necessary to extend the invitation to participate to a total of 1,943 employees.
The logistics of data collection meant that an average of 40 workers could be evaluated each day. To reach the required total figure, approximately 49 days of evaluation would be needed. Taking into account that there are 20 working days in a month (from Monday to Friday), the total duration of the recruitment and data collection period extended over about 3 months.
Definition of variables
The main variable in this study was obesity, and it was decided to measure it using bioimpedance as a reference test. Bioimpedance is a non-invasive technique that estimates body composition, including body fat, by measuring the body’s electrical resistance. This resistance is inversely proportional to the body’s water content, which in turn is related to fat mass and fat-free mass.
Bioimpedance has several advantages. Firstly, it is a non-intrusive procedure, implying it does exclude penetration or slicing of the body or presentation to radiation, making it more reasonable to members contrasted with other strategies for example computed tomography. Second, it is speedy and easy-to-use, permitting assessment of an extensive number of individuals in a brief time period. Third, despite the fact that resistance is not as precise as computed tomography for estimating fat bulk, it has appeared to be moderately exact and dependable in gauging fat in expansive and different populaces, making it appropriate for this examination [10]. For this examination, obesity was considered if the extent of fat was more prominent than 25% in males and 35% in females [11].
The anthropometric measures tested were: WC; BMI = weight (kg)/height2 (m); WHtR = WC/height; tri-ponderal mass index (TMI) = weight (kg)/height3 (m) [12]; new BMI = 1.3 × (weight (kg)/height (m)2.5) [13, 14]; Clinica Universidad de Navarra-Body Adiposity Estimator (CUN-BAE)men = -44.988 + (0.503 × age) + (10.689 × 0) + (3.172 × BMI) - (0.026 × BMI2) + (0.181 × BMI × 0) - (0.02 × BMI × age) - (0.005 × BMI2 × 0) + (0.00021 × BMI2 × age) [15]; CUN-BAEwomen = -44,988 + (0.503 × age) + (10.689 × 1) + (3.172 × BMI) - (0.026 × BMI2) + (0.181 × BMI × 1) - (0.02 × BMI × age) - (0.005 × BMI2 × 1) + (0.00021 × BMI2 × age) [15]; waist BMI (wBMI) = weight × WC/height2 [16].
Different variables were adopted from the workers in the course of the research. Even though these extra variables were not instantly used in the diagnostic accuracy analyses, they were incorporated to better comprehend the illustrative attributes of worker people. These were demographic data like age and gender; behavioral data like tobacco and alcohol consumption; and occupational data like the sort of labor.
Data collection and procedure
The evaluation process at the medical center is described as follows. Upon arrival at the clinic, every worker receives a letter at the reception, which they sign to confirm the accuracy of all the information offered. They are given a form to finish with their personal medical history. Subsequently, the workers are directed to the nursing team. Here, different measurements are taken. Height is resolved utilizing an anthropometer, and weight is listed using an electronic scale, ensuring that topics are in light garments for an accurate reading. Waist girth is computed by employing a measuring tape, with the individual in an upright position, bare torso, and feet spaced between 25 and 30 cm apart, at the level of the superior border of the iliac crest.
All these data are recorded in the worker’s medical history. At this point, the principal investigator introduced themselves and provided informed consent, clarifying the purpose of the study, and if the worker agreed, proceeded to measure body fat using bioimpedance. For this, the TBF-300A body composition analyzer (TANITA Corporation, Tokyo, Japan) was used. Measurements were performed according to the manufacturer’s specifications. The average taking time was 4 min.
Continuing with the classic routine, the worker is directed to the laboratory. The staff verifies that the worker has met the requirement of at least 8 h of fasting. Then, a 5 mL blood sample is taken through venipuncture. Finally, they are taken to the medical office for a medical evaluation. This evaluation consists of several parts: initially, the occupational physician asks about the worker’s biological, pathological, and family history. This is followed by a physical examination and a musculoskeletal examination, during which questions about physical activity practice are asked. Depending on the individual’s type of work, additional examinations may be performed. All data collected during this evaluation are noted in the worker’s medical history.
Statistical analysis
Statistical analyses were performed using R software version 4.0.5. First, a descriptive analysis was developed, summarizing categorical variables in absolute terms and percentages, and numerical variables using the mean and standard deviation (SD).
The diagnostic capability of the markers was evaluated using the area under the receiver operating characteristic (ROC) curves (AUCs). The diagnostic property of the cutoff values for obesity was assessed with the Youden index (sensitivity + specificity - 1). Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (LR+), and negative likelihood ratio (LR-) were calculated. Analyses were stratified by sex and presented with their respective 95% confidence intervals (95% CIs). All analyses were presented stratified by sex.
Ethical considerations
The protocol was approved by the ethics committee of the Faculty of Medicine at Ricardo Palma University (PG 081 2023). Permission was also obtained from the clinic. To ensure participants’ anonymity, no personal data (such as names, identity document numbers, etc.) were requested. Additionally, the database was handled only by the principal investigator.
Each worker was given the consent form. Participants who agreed had to mark the option “I have read the consent form and agree with it.” The entire research process was carried out in compliance with the Helsinki Declaration.
| Results | ▴Top |
In our analysis, 780 individuals participated, categorized by gender. According to the study, the overall obesity rate amounted to 19.74%, with the rate among male and female participants being 18.00% and 21.25%, respectively. Age group circulation displayed variance, with a higher percentage of overweight males in the 18 to 29 year band (36.67%) and a more balanced distribution in other age bands. Regarding occupational diversity, male operators showed a higher fraction of non-obesity (82.28%) compared to administrative staff (81.73%). Alcohol intake revealed that 93.33% of males who consumed alcohol were not overweight, while daily tobacco intake showed that 90.74% of male smokers were not overweight. Those additional calculations revealed that non-overweight males, on average, had a BMI of 24.4 (4.3) while overweight males averaged 30.1 (6.1), with non-overweight males having a normal waist span of 92 (12) cm compared to the 104 (9) cm waist span of overweight males. For a detailed overview of the remaining outcomes, please refer to Table 1.
 Click to view | Table 1. Characteristics of the Study Sample Distributed According to Obesity and Sex |
Figure 1 illustrates how the proportion of internal body fat determined by bioimpedance concerning each evaluated bodily measure.
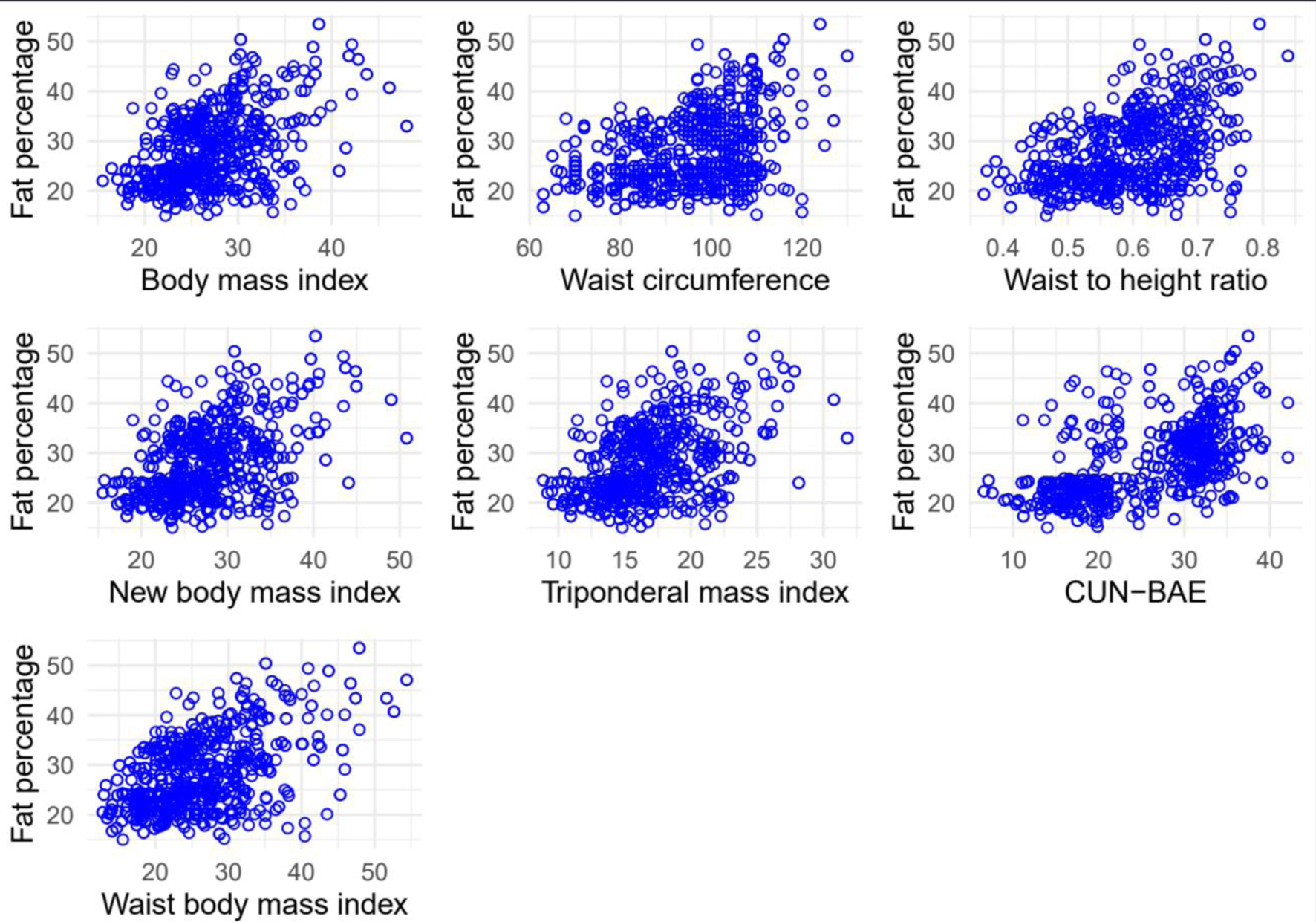 Click for large image | Figure 1. Scatter plot between the percentage of fat and each anthropometric marker evaluated. |
In terms of the analytic assessment for rating excess weight, the measure with the greatest accuracy in women proved to be wBMI with an AUC of 0.783 (95% CI: 0.735 - 0.830), demonstrating a sensitivity of 71.59% (95% CI: 60.98 - 80.69) and a specificity of 74.54% (95% CI: 69.45 - 79.18). For males, wBMI represented the most accurate measure and produced an AUC of 0.828 (95% CI: 0.779 - 0.878), a sensitivity of 89.39% (95% CI: 79.36 - 95.62), and a specificity of 58% (95% CI: 52.19 - 63.65). Additional results are available in Table 2 and visually represented in Figure 2.
 Click to view | Table 2. Diagnostic Values of Antropometric Measures for Obesity |
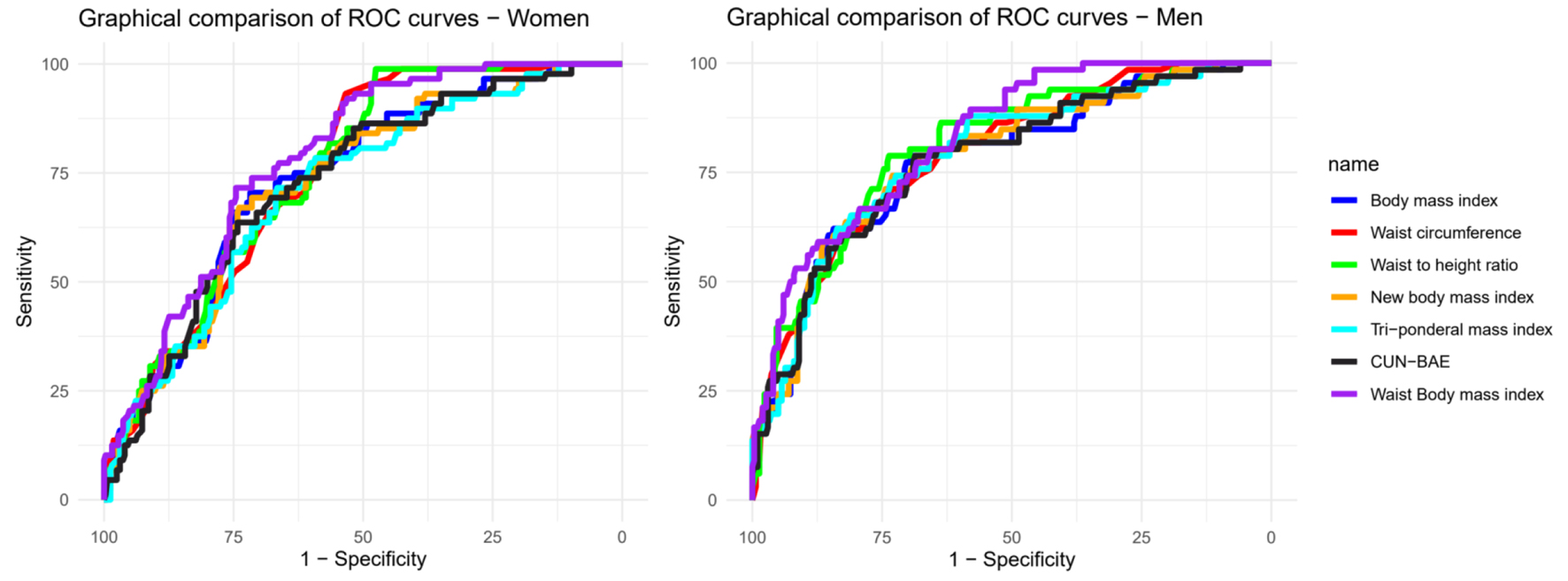 Click for large image | Figure 2. Graph of ROC curves between the percentage of fat and each anthropometric marker evaluated stratified by sex. ROC: receiver operating characteristic. |
| Discussion | ▴Top |
Main findings
Among all these signs, we found that wBMI, adopted by WHtR, proved to be the most accurate method for diagnosing obesity. This discovery indicates that traditional markers like BMI are not the most acceptable markers compared to others in assessing obesity status. It also reflects the possibility to offer an powerful and accessible instrument in the prevention and management of this widespread health situation.
Comparison with other studies
BMI remains an advisable health worthfulness measurement tool by the World Health Organization [11]. Nevertheless, its correctness is limited, especially in citizens with oversized muscle mass like athletes, and its utility is not correctly changed for gender. What’s more, BMI does not provide information about how body fat is spread out, a critical factor in obesity appraisal. Accordingly, WC has gained admittance as an indispensable clinical sign for the unstraightforward appraisal of the obesity, particularly when it is visceral and concentrated in the abdomen [7].
When it comes to WHtR, its usefulness goes beyond simple obesity detection and has shown to be a strong forecaster of heart and metabolism risk. A study by Ashwell and Gibson [17] suggests WHtR is a better and more overall indicator of heart and metabolism disease risk than BMI. These results were supported by Lu et al. Moreover, other studies have found a good connection between WHtR and the development of illnesses like T2DM [18, 19] or hypertension [20].
About wBMI, the best indicator of obesity according to our final results, there are not much data accessible up to now, as it is a lately used indicator. Initially, this index was formerly proposed to predict abnormal cardiac structure, insulin resistance, increased arterial stiffness, and dyslipidemia [16]. The work of Moltrer et al [21] came to identical completion as our investigation, pointing out the superiority of this new indication over the rest.
The superiority of wBMI as a diagnostic resource for obesity can be attributed to a small number of circumstances. Initially, wBMI takes into account stature, heaviness, and WC. This renders a more precise picture of body fat allocation in contrast to measures that consider only one of these circumstances. In comparison, BMI, for example, only considers weight in relation to height, leading to underestimation or exaggeration of obesity in tall or short persons, correspondingly [17, 22]. And even though WHtR combines stature and WC, merging it with load seems to be a much superior tactic.
Additionally, this presents greater specificity in women than in men, which may be due to inherent biological differences in the distribution of body fat between males and females. Traditionally, women tend to accumulate more fat in the hip and thigh regions, while men typically accumulate it in the abdominal area. These differences can influence the accuracy of various anthropometric measurements for diagnosing obesity. The wBMI, by taking into account WC as well as weight and height, could be better capturing these body fat distribution differences and, therefore, providing a more accurate assessment of obesity risk and related conditions across genders [23].
It is important to note that the limit of detail we chose for WHtR is 0.59, which is noticeably higher than the historic limit point of 0.5, and has historically used to pinpoint cardiovascular risk [24]. This difference might reflect disparities in excess weight allotment and body morphology among different populations. Although our limit detail is higher, the writers accept that it offers a more exact representation of obesity in the study crowd. In turn, numerous studies use the limit point of 0.5 to specify obesity, which may result in an overestimation of the percentage of overweight persons, often achieving up to 80% [25]. This is a significant number and could divert attention from public health strategies and resource allocation to individuals who may not have a real risk of building obesity-related comorbidities. In this sense, careful assortment of the limit point for WHtR is crucial to avoid excessive diagnoses and ensure efficient use of healthcare resources.
It is crucial to emphasize that the limits applied to outline obesity, whether by BMI or WC, may vary from standard or global cutoff points. These divergences can materialize owing to variations in physical composition, heredity, and external elements among diverse groups. Global cutoff points may not apply to all populations and might result in overestimation or underestimation of obesity occurrence. Thus, it is important to figure out and use population-specific cutoff points to accomplish an accurate assessment of obesity standing. This is fundamental to ensure proper diagnosis, the execution of effective public health interventions, and the efficient allotment of healthcare resources.
Public health importance
The findings of this analysis have considerable effects for populace wellbeing. To start with, they demonstrate that wBMI may be a more exact gauge for diagnosing obesity compared to other commonly used steps. This signifies that few cases of adiposity would go unnoticed, letting early intercession. In this manner, it would have a sizable influence on the competence and precision of wellbeing evaluations in various clinical and community settings.
Moreover, wBMI is a straightforward step that can be readily utilized in the world of everyday clinical practice, without requiring costly machinery or expert coaching. This makes it particularly valuable in settings with restricted access to advanced diagnostic exams.
In the end, the effectiveness of wBMI in discovering excess weight can assist in bettering avoidance and therapy tactics. By accurately distinguishing overweight persons, health care professionals are better able to guide interventions to forestall connected long-term health issues like diabetes and cardiovascular problems. This has the potential to yield more advantageous consequences in the long run, lessened expenses related to medical care, and an elevated standard of living for those individuals.
Study limitations
Possible limitations of our study include: first, although the decision to use the bioimpedance method is explained in the methods section, it is not the gold standard. Second, the cutoff point used to define obesity according to the reference test, as an appropriate population-level limit has not been established. Third, the sample used has been in workers from a specific place, which could distance us from the probability of extrapolating it to a broader level.
Conclusions
Our work finishes that wBMI proved to be a superior instrument for diagnosing obesity compared to traditional measures such as BMI, WC, WHtR, and other evaluated anthropometric measurements. This superiority lies in its capability to include data about body fat allocation, an essential factor regularly disregarded by other steps.
These discoveries, together with its simplicity and ease of use, make wBMI a valuable instrument for use in medical and public health contexts. It is vital that further research be directed to corroborate and extend our discoveries in different populations and contexts. Additionally, it will be critical to explore how wBMI can be successfully incorporated into clinical practice rules and public health structures. This will enable us optimize its effect on population health.
If the outcomes are validated, its broad dissemination is expected to advance the correctness of obesity conclusion, allow for more timely and prosperous protective interventions, and lend a hand to more effectual government of the obesity epidemic and its affiliated comorbidities.
Acknowledgments
We extend our gratitude to the dedicated team of doctors, nurses, and technicians at the polyclinic for their unwavering support throughout our research journey.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Informed consents have been obtained from participants.
Author Contributions
Conceptualization: Victor Juan Vera-Ponce, Joan A. Loayza-Castro. Project design: Fiorella E. Zuzunaga-Montoya, Luisa Erika Milagros Vasquez-Romero, Willy Ramos, Mario J. Valladares-Garrido. Data collection: Fiorella E. Zuzunaga-Montoya, Cori Raquel Iturregui Paucar. Formal analysis: Victor Juan Vera-Ponce. Research: Luisa Erika Milagros Vasquez-Romero, Joan A. Loayza-Castro. Methodology: Victor Juan Vera-Ponce. Project administration: Victor Juan Vera-Ponce. Resources: Jhony A. De La Cruz-Vargas. Software: Victor Juan Vera-Ponce. Supervision: Jhony A. De La Cruz-Vargas. Writing - original draft: Victor Juan Vera-Ponce, Luisa Erika Milagros Vasquez-Romero, Cori Raquel Iturregui Paucar, Mario J. Valladares-Garrido, Willy Ramos, Norka Rocio Guillen Ponce, Jhony A. De La Cruz-Vargas. Writing - review and editing: Fiorella E. Zuzunaga-Montoya, Joan A. Loayza-Castro, Cori Raquel Iturregui Paucar, Mario J. Valladares-Garrido, Willy Ramos, Norka Rocio Guillen Ponce, Jhony A. De La Cruz-Vargas.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- World Obesity Day Atlases | Obesity Atlas 2022 [Internet]. World Obesity Federation Global Obesity Observatory. [citado el 19 de junio de 2023]. Disponible en: https://data.worldobesity.org/publications/?cat=15.
- Bluher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15(5):288-298.
doi pubmed - Ruze R, Liu T, Zou X, Song J, Chen Y, Xu R, Yin X, et al. Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Front Endocrinol (Lausanne). 2023;14:1161521.
doi pubmed pmc - Kumanyika S, Dietz WH. Solving population-wide obesity - progress and future prospects. N Engl J Med. 2020;383(23):2197-2200.
doi pubmed - Romero-Corral A, Somers VK, Sierra-Johnson J, Thomas RJ, Collazo-Clavell ML, Korinek J, Allison TG, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes (Lond). 2008;32(6):959-966.
doi pubmed pmc - Ashwell M. Obesity risk: importance of the waist-to-height ratio. Nurs Stand. 2009;23(41):49-54.
doi pubmed - Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, Santos RD, et al. Waist circumference as a vital sign in clinical practice: a Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16(3):177-189.
doi pubmed pmc - Chan DC, Watts GF, Barrett PH, Burke V. Waist circumference, waist-to-hip ratio and body mass index as predictors of adipose tissue compartments in men. QJM. 2003;96(6):441-447.
doi pubmed - Cohen JF, Korevaar DA, Altman DG, Bruns DE, Gatsonis CA, Hooft L, Irwig L, et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: explanation and elaboration. BMJ Open. 2016;6(11):e012799.
doi pubmed pmc - Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gomez J, Lilienthal Heitmann B, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004;23(6):1430-1453.
doi pubmed - Physical status: the use and interpretation of anthropometry. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser. 1995;854:1-452.
pubmed - Peterson CM, Su H, Thomas DM, Heo M, Golnabi AH, Pietrobelli A, Heymsfield SB. Tri-ponderal mass index vs body mass index in estimating body fat during adolescence. JAMA Pediatr. 2017;171(7):629-636.
doi pubmed pmc - New BMI (New Body Mass Index) [Internet]. [citado el 29 de mayo de 2022]. Disponible en: https://people.maths.ox.ac.uk/trefethen/bmi.html.
- Van Haute M, Rondilla E, 2nd, Vitug JL, Batin KD, Abrugar RE, Quitoriano F, Dela Merced K, et al. Assessment of a proposed BMI formula in predicting body fat percentage among Filipino young adults. Sci Rep. 2020;10(1):21988.
doi pubmed pmc - Ares Blanco J, Valdes Hernandez S, Botas Cervero P, Sanchez-Ragnarsson C, Pujante Alarcon P, Menendez-Torre E, Delgado Alvarez E. Estimation of body fat mass using the CUN-BAE index and mortality risk by sex in the Asturias Study cohort. Endocrinol Diabetes Nutr (Engl Ed). 2019;66(8):487-494.
doi pubmed - Antonini-Canterin F, Di Nora C, Poli S, Sparacino L, Cosei I, Ravasel A, Popescu AC, et al. Obesity, cardiac remodeling, and metabolic profile: validation of a new simple index beyond body mass index. J Cardiovasc Echogr. 2018;28(1):18-25.
doi pubmed pmc - Ashwell M, Gibson S. Waist to height ratio is a simple and effective obesity screening tool for cardiovascular risk factors: Analysis of data from the British National Diet And Nutrition Survey of adults aged 19-64 years. Obes Facts. 2009;2(2):97-103.
doi pubmed pmc - Zhang FL, Ren JX, Zhang P, Jin H, Qu Y, Yu Y, Guo ZN, et al. Strong Association of Waist Circumference (WC), Body Mass Index (BMI), Waist-to-Height Ratio (WHtR), and Waist-to-Hip Ratio (WHR) with diabetes: a population-based cross-sectional study in Jilin Province, China. J Diabetes Res. 2021;2021:8812431.
doi pubmed pmc - Chen N, Hu LK, Sun Y, Dong J, Chu X, Lu YK, Liu YH, et al. Associations of waist-to-height ratio with the incidence of type 2 diabetes and mediation analysis: Two independent cohort studies. Obes Res Clin Pract. 2023;17(1):9-15.
doi pubmed - Li Y, Gui J, Zhang X, Wang Y, Mei Y, Yang X, Liu H, et al. Predicting hypertension by obesity- and lipid-related indices in mid-aged and elderly Chinese: a nationwide cohort study from the China Health and Retirement Longitudinal Study. BMC Cardiovasc Disord. 2023;23(1):201.
doi pubmed pmc - Moltrer M, Pala L, Cosentino C, Mannucci E, Rotella CM, Cresci B. Body mass index (BMI), waist circumference (WC), waist-to-height ratio (WHtR) e waist body mass index (wBMI): Which is better? Endocrine. 2022;76(3):578-583.
doi pubmed - Han TS, Seidell JC, Currall JE, Morrison CE, Deurenberg P, Lean ME. The influences of height and age on waist circumference as an index of adiposity in adults. Int J Obes Relat Metab Disord. 1997;21(1):83-89.
doi pubmed - Chen Y, Zhang Z, Wang J, Sun H, Zhao X, Cheng X, Zhao Q. Sex differences in the association of abdominal adipose tissue and anthropometric data with untreated hypertension in a Chinese population. Biol Sex Differ. 2020;11(1):38.
doi pubmed pmc - Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr Res Rev. 2010;23(2):247-269.
doi pubmed - Paz-Krumdiek M, Rodriguez-Velez SG, Mayta-Tristan P, Bernabe-Ortiz A. Association between sitting time and obesity: A population-based study in Peru. Nutr Diet. 2020;77(2):189-195.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
