| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Case Report
Volume 8, Number 2-3, May 2018, pages 43-46
Abdominal Pain in Diabetic Ketoacidosis: Beyond the Obvious
Carlos Tavares Belloa, c, Miguel Franco Gagob, Francelina Fernandesb, Maria Manuela Oliveiraa
aDepartment of Endocrinology, Hospital de Egas Moniz, Rua da Junqueira 126, 1349-019 Lisboa, Portugal
bDepartment of Radiology, Hospital de Egas Moniz, Rua da Junqueira 126, 1349-019 Lisboa, Portugal
cCorresponding Author: Carlos Tavares Bello, Department of Endocrinology, Hospital de Egas Moniz, Rua da Junqueira 126, 1349-019 Lisboa, Portugal
Manuscript submitted March 3, 2018, accepted March 21, 2018
Short title: Abdominal Pain in Diabetic Ketoacidosis
doi: https://doi.org/10.14740/jem494w
| Abstract | ▴Top |
Diabetic ketoacidosis (DKA) is a medical emergency characterized by hyperglycemia, high anion gap metabolic acidosis and elevated circulating ketone bodies resulting from severe impairment of insulin secretion and/or action. Besides dehydration, nausea and vomiting, abdominal pain is also considered to be a cardinal clinical feature of DKA. Diagnosis relies on biochemical criteria, and disease severity on clinical and laboratory findings. Radiological investigation is not standard of care of DKA despite being required in specific situations. The authors report on a case of a patient with DKA and abdominal pain, whose investigation revealed chronic pancreatitis and a massive splenic artery pseudoaneurysm. The case is remarkable for the rarity of the clinical entity and reminds the clinician to the importance of imaging in newly diagnosed diabetes.
Keywords: Abdominal pain; Diabetic ketoacidosis; Chronic pancreatitis; Splenic artery pseudoaneurysm
| Introduction | ▴Top |
Diabetic ketoacidosis (DKA) is a frequent medical emergency with a rising incidence [1]. It accounts for 14% of all hospital admissions of diabetic patients [2]. Diagnosis relies on biochemical criteria, which include hyperglycemia (blood glucose > 250 mg/dL), high anion gap metabolic acidosis (bicarbonate < 18 mmol/L and anion gap > 10 mmol/L) and elevated blood ketone bodies (> 3 mmol/L) [3]. Patients often present to the emergency department reporting polyuria, polydipsia, weight loss, weakness, nausea, vomiting and abdominal pain of recent onset. Physical examination is typically remarkable for signs of dehydration, tachycardia, hypotension and tachypnea with acetonic breath. Severity is determined by blood gas findings (pH, serum bicarbonate, and anion gap), urine/blood ketone body levels, serum osmolality and mental status changes [3].
Abdominal pain is a frequent DKA manifestation (present in 40-75% of the cases) and its prevalence increases as arterial pH and serum bicarbonate levels decline. Furthermore, abdominal rebound tenderness, suggesting the presence of an acute abdomen, affects 12% of DKA patients with abdominal pain [4]. Many mechanisms have been suggested to underlie the abdominal symptoms in DKA, namely acute hyperglycemia mediated impaired gastrointestinal motility (esophageal, gastric and gallbladder), rapid expansion of the hepatic capsule, and mesenteric ischemia precipitated by volume depletion. Although metabolic stabilization by itself often results in clinical improvement, in up to 35% of the patients, the precipitant of DKA is the underlying etiology of the abdominal pain (pancreatitis, hepatitis, pyelonephritis, pelvic inflammatory disease, and gastritis) and surgery is warranted in 6% of the cases (Fournier’s necrotizing fasciitis, acute cholecystitis, appendicitis and perineal abscess) [4].
Chronic pancreatitis is a recognized cause of diabetes mellitus (DM). It occurs in the late course of chronic pancreatitis and has an estimated prevalence of 70% [5]. Despite being associated with severe insulin deficiency, DKA is unusual as alpha cell secretory function is also severely compromised [6]. Apart from DM, chronic pancreatitis has also been associated with additional complications, namely pseudocyst formation, pancreatic fistula, ascites, steatorrhea and splenic artery pseudoaneurysms. As the latter are exceedingly rare, despite usually being symptomatic and life-threatening, imaging investigations in the setting of a DKA or acute pancreatitis are virtually never pseudoaneurysm-directed.
The authors report on a case of a patient presenting with DKA that arose in the setting of chronic pancreatitis, whose imaging investigation revealed a splenic artery pseudoaneurysm.
| Case Report | ▴Top |
The authors report on a 41-year-old male patient with past medical history of active smoking and recurrent episodes of acute alcoholic pancreatitis that presented to the emergency department with abdominal pain, nausea and vomiting of sudden onset for the past 24 h. The patient also reported polyuria, polydipsia and 16 kg weight loss (23% of initial body weight) for the last 4 weeks, and his current body mass index was 20 kg/m2.
Upon admission, the patient was calm, oriented in time, space and person, tachycardic (120 beats per minute), normotensive (supine blood pressure of 111/77 mm Hg) and hyperglycemic (capillary blood glucose of 600 mg/dL).
Blood ketone levels were high (5.1 mmol/L) and arterial blood gases revealed high anion gap metabolic acidosis (pH 7.42, bicarbonate 17.9 mmol/L, anion gap of 21 mmol/L, and glucose 601 mg/dL). Laboratory investigation is represented on Table 1.
 Click to view | Table 1. Admission Laboratory Parameters |
Intravenous saline and insulin administration led to rapid clinical and biochemical improvement, rendering the patient normoglycemic and asymptomatic within 5 h. As no obvious precipitating event was identified, anti-insulin, islet cell, GAD65 and ZnT8 antibodies were requested, being all undetectable.
Due to the history of alcohol abuse, slight elevation of serum lipase and severity of the abdominal pain, the patient underwent abdominal ultrasound that documented a homogeneous hepatomegaly, pancreatic enlargement (with diffuse punctate calcifications), a pancreatic pseudocyst of the pancreatic head and a splenic artery pseudoaneurysm (Fig. 1). Contrast-enhanced CT of the abdomen further confirmed the splenic artery pseudoaneurysm with 47 × 47 × 61 mm and two pancreatic pseudocysts with 28 and 21 mm (Fig. 2).
 Click for large image | Figure 1. Abdominal ultrasound: enlarged pancreas with diffuse calcifications suggestive of chronic pancreatitis. There is a bulky aneurysmatic vascular lesion with a mural thrombus, located in the superior aspect of the pancreatic tail that seems to stem from the splenic artery. |
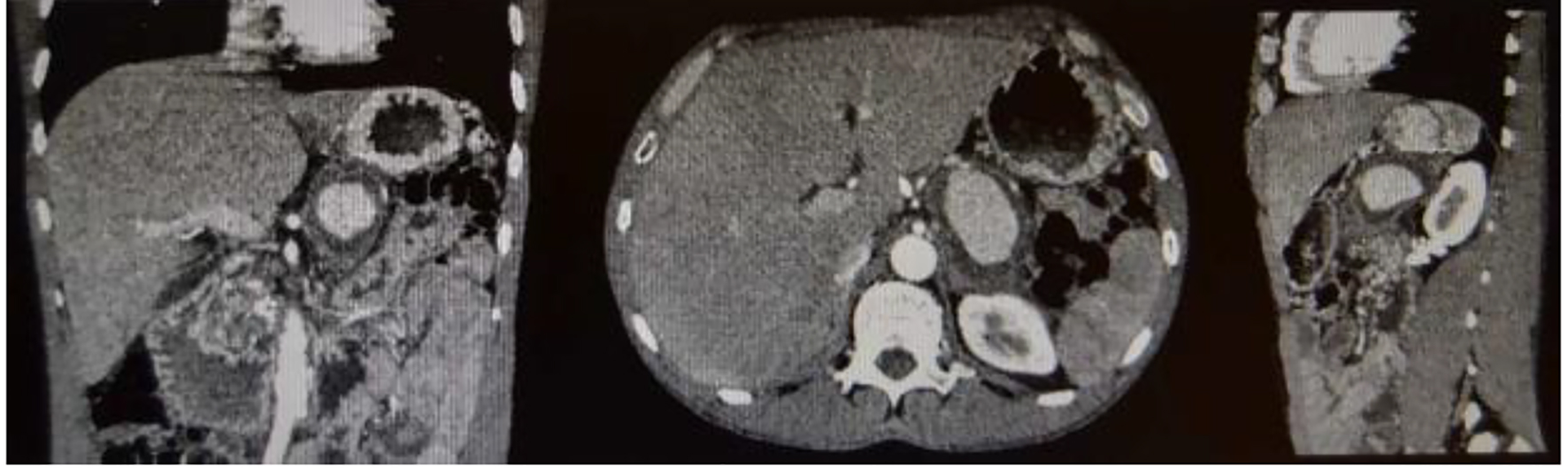 Click for large image | Figure 2. Contrast-enhanced abdominal CT scan. There is an evident aneurysmal vascular lesion with at least 68 mm of longer axis, exhibiting a mural thrombus, closely related with the splenic artery, which is located antero-superiorly. It enhances less intensely in the dominant arterial phase compared to the branches of the celiac trunk. Its probable starting point is the splenic artery, given its topography and clinical context. The Doppler color coding with YingYang signal also indicates that it is an arterial structure. |
Due to the large size and significant surgical risk, the patient underwent pseudoaneurysm coiling, which was uneventful. DM was adequately controlled with a basal-bolus insulin regimen, remarkable for high prandial insulin requirements.
Currently, the patient is well, has stopped drinking alcohol, is adherent to the intensive insulin regimen and reports no additional abdominal complaints.
| Discussion | ▴Top |
Splenic artery pseudoaneurysms are rare clinical entities, with less than 200 cases described in the English literature [7]. In contrast with true aneurysms, pseudoaneurysm wall consists of intima and media layers without any overlying adventitia [8]. It may be caused by pancreatitis, trauma, peptic ulcer disease and surgical damage. Recurrent episodes of pancreatitis are associated with splenic artery necrotizing arteritis, which is considered to be the underlying cause of vessel wall damage that leads to pseudoaneurysm formation [7]. Patients are often symptomatic (97.5% of the cases) and present with abdominal pain (29.5%), hematochezia or melena (26.2%), hematemesis (14.8%) or hemorrhage into the pancreatic duct (20.3%) [8]. Timely recognition and intervention are crucial in order to prevent rupture (that occurs in 37% of the cases) which carries a high mortality rate (90%) [9, 10]. As such, treatment is always indicated and should be scheduled as soon as possible. Lesion excision along with splenectomy and/or partial pancreatectomy when indicated is considered the treatment of choice. The latter is unfortunately associated with high mortality and morbidity rate (1.3% and 9%, respectively) [11]. Endovascular approaches (coils, detachable balloons, inert particles or gelatin sponge), due to their lower theoretical operative risk, are increasingly being employed despite having a slightly lower success rate (75-85%) [11].
Additional complications of pancreatitis include the pseudocyst formation, as seen in the reported case, that usually heralds a previous episode of acute pancreatitis within the last 8 weeks [12]. No therapy is indicated unless significant space occupying effects or symptoms emerge [13].
Although DM is a frequent complication of established chronic pancreatitis, it rarely presents with DKA [6]. The latter is usually precipitated by infectious diseases (40%), insulin therapy non-compliance (25%) and newly diagnosed DM (15%, mostly type 1 DM) [2]. The investigation of the underlying cause of the DKA is of utmost importance since it is the major determinant of patient mortality [3]. Acute cardiovascular events, sepsis and acute pancreatitis must be actively excluded [3]. If no evidence of such events is identified, a DKA in the setting of new onset DM (usually type 1) can eventually be diagnosed. However, Thomas et al, using UK Biobank data have recently challenged the designation of type 1 DM as juvenile diabetes, by proving that 47% of new onset type 1 DM cases are diagnosed after the third decade of life [14]. Since the reported patient did not have the diagnosis of chronic pancreatitis at admission, presented with DKA, had no significant elevation of serum lipase and rapidly improved after metabolic compensation, imaging investigation could have been easily considered optional. This is a typical presentation of new onset type 1 DM, which presents with DKA in up to 25% of adult cases [15]. However, none of the type 1 DM autoantibodies were detected, arguing against the type 1 DM diagnosis. The history of recurrent episodes of acute pancreatitis and alcohol abuse was the reason for abdominal imaging in the reported case. No obvious pulsating abdominal mass was detected on physical examination despite its large dimensions. The authors consider that the finding of the pseudoaneurysm was completely incidental and unrelated to the abdominal symptoms that arose in the setting of the DKA, but its finding has been crucial and probably lifesaving in this particular patient with risk factors for pseudoaneurysm formation.
The approach to a patient with DKA must be holistic and should integrate all patients’ comorbidities. The diagnosis of the precipitating event has to be actively pursued and exclusive metabolic compensation should be avoided in order to optimize patient care in the acute and long term setting.
Conclusions
1) DM is a frequent complication of established chronic pancreatitis.
2) Pancreatogeneous diabetes may present with DKA.
3) Splenic artery pseudoaneurysms are rare complications of pancreatitis being less than 200 cases described in the English language literature so far.
4) Pseudoaneurysms are often symptomatic and have a high rupture risk if left undiagnosed and untreated.
5) A holistic approach to a patient with DKA is warranted in order to optimize patient outcomes.
Conflict of Interest
The authors have no conflict of interest to declare.
| References | ▴Top |
- Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32(7):1335-1343.
doi pubmed - Diabetic Ketoacidosis: Emedicine.medscape.com. 2017. Available from: http://emedicine.medscape.com/article/118361-overview#a6.
- Umpierrez G, Korytkowski M. Diabetic emergencies - ketoacidosis, hyperglycaemic hyperosmolar state and hypoglycaemia. Nat Rev Endocrinol. 2016;12(4):222-232.
doi pubmed - Umpierrez G, Freire AX. Abdominal pain in patients with hyperglycemic crises. J Crit Care. 2002;17(1):63-67.
doi pubmed - Wang W, Guo Y, Liao Z, Zou DW, Jin ZD, Zou DJ, Jin G, et al. Occurrence of and risk factors for diabetes mellitus in Chinese patients with chronic pancreatitis. Pancreas. 2011;40(2):206-212.
doi pubmed - Ewald N, Hardt PD. Diagnosis and treatment of diabetes mellitus in chronic pancreatitis. World J Gastroenterol. 2013;19(42):7276-7281.
doi pubmed - Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. AJR Am J Roentgenol. 2007;188(4):992-999.
doi pubmed - Tessier DJ, Stone WM, Fowl RJ, Abbas MA, Andrews JC, Bower TC, Gloviczki P. Clinical features and management of splenic artery pseudoaneurysm: case series and cumulative review of literature. J Vasc Surg. 2003;38(5):969-974.
doi - Huang IH, Zuckerman DA, Matthews JB. Occlusion of a giant splenic artery pseudoaneurysm with percutaneous thrombin-collagen injection. J Vasc Surg. 2004;40(3):574-577.
doi pubmed - LiPuma JP, Sachs PB, Sands MJ, Stuhlmiller S, Herbener TE. Angiography/interventional case of the day. Splenic artery pseudoaneurysm associated with pancreatitis. AJR Am J Roentgenol. 1997;169(1):259, 262-253.
- Guillon R, Garcier JM, Abergel A, Mofid R, Garcia V, Chahid T, Ravel A, et al. Management of splenic artery aneurysms and false aneurysms with endovascular treatment in 12 patients. Cardiovasc Intervent Radiol. 2003;26(3):256-260.
doi pubmed - Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol. 2009;15(1):38-47.
doi pubmed - Pujahari AK. Chronic Pancreatitis: A Review. Indian J Surg. 2015;77(Suppl 3):1348-1358.
doi pubmed - Half of all type 1 diabetes develops after 30 years of age [Internet]. Medscape. 2017. Available from: http://www.medscape.com/viewarticle/869028#vp_2.
- McCulloch David K. Clinical presentation and diagnosis of diabetes mellitus in adults. 2017.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
