| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Case Report
Volume 4, Number 4, August 2014, pages 112-114
Chronic Active Epstein-Barr Virus Infection Mimicking Diabetic Ketoacidosis
Vishwanath Pattana, Nilma Malika, Waqas Jehangira, b, Noureen Jassania, Hongxio Luoa, Purnendu Sena, Abdalla Yousifa
aDepartment of Internal Medicine, Raritan Bay Medical Center, Perth Amboy, NJ, USA
bCorresponding Author: Waqas Jehangir, 530 New Brunswick Ave, Perth Amboy, NJ 08861, USA
Manuscript accepted for publication July 25, 2014
Short title: Chronic Active Epstein-Barr Virus
doi: https://doi.org/10.14740/jem230w
| Abstract | ▴Top |
Epstein-Barr virus (EBV) is a widely disseminated herpes virus that spreads by intimate contact between susceptible person and symptomatic EBV shedders. Most patients recover without complications. Chronic active Epstein-Barr virus (CAEBV) infection is a very rare complication of EBV in which previously healthy persons develop severe, life-threatening illness. We report a rare case of a CAEBV infection in a 20-year-old female mimicking a common clinical presentation of diabetic ketoacidosis.
Keywords: Epstein-Barr virus infection; Diagnostic dilemma; Diabetic ketoacidosis
| Introduction | ▴Top |
Primary Epstein-Barr virus (EBV) infection is rare in first year of life, relatively benign in childhood and has high incidence of infectious mononucleosis and complications in late adolescence and adulthood. The majority of patients with infectious mononucleosis recover without apparent sequelae, and mortality is very rare. However, severe neurologic complications can occur in 1-5% patients (transverse myelitis, meningoencephalitis, cerebellitis) and death can occur with splenic rupture (0.5-1% cases), airway obstruction (about 1% cases) or very rarely in male patients with X-linked lymphoproliferative syndrome [1]. Chronic active Epstein-Barr virus (CAEBV) infection is a very rare cause of mortality which can be missed because of its rare occurrence and limited literature describing its natural course and characteristics. CAEBV in adults manifests mostly as fever, fatigue and lymphadenopathy with an uncertain clinical course but can be lethal. It reactivates with moderately high antibody titers of viral capsid antigen (VCA) IgG and EA IgG and with low antibody titers to EBV nuclear antigen (EBNA) [2].
| Case Report | ▴Top |
A 20-year-old Caucasian female was admitted to hospital because of lightheadedness and progressively worsening shortness of breath. Two weeks prior to admission she started having easy fatigability followed by polyuria and polydipsia for 3 days. Patient denied fever, sore throat, sick contacts, recent travel or loss of appetite and any significant past medical or surgical history. She was sexually active with single male partner with safe sex practice for the last 6 months.
On admission patient had pulse rate 138/min, BP 195/145 mm Hg, RR 40/min, oxygen saturation 90% on room air and temperature 97.6 °F (36.4 °C). On examination patient was lethargic and in respiratory distress had pale conjunctiva, clear lung fields, regular tachycardia without third or fourth heart sounds and no murmurs. Her lab data showed hemoglobin 8.7 g/dL, WBC 37,800/mm3 (26% neutrophils, 12% bands, 50% lymphocytes and 2% atypical lymphocytes). Glucose 347 mg/dL, bicarbonate 7 mEq/L, anion gap 25 mEq/L, BUN 29 mg/dL and creatinine 2.9 mg/dL. Her urine was negative for pregnancy, ketones and drug screen. ABG showed pH 7.28, PCO2 17.4 mm Hg, PO2 60.8 mm Hg, oxygen saturation 86% on 35% FiO2. Her EKG was normal and portable chest X-ray showed no infiltrates. Patient was treated with IV insulin drip for suspected diabetic ketoacidosis with cautious fluid management because of possible cardiomegaly on portable chest X-ray and positive troponins (0.66 ng/mL). However, subsequent HbA1c value was 5.6 and serum ketone was negative. Within 12 h of admission patient, however, deteriorated rapidly and died of cardio-respiratory arrest secondary to severe systolic heart failure. Review of imaging record for accidental sports-related injury 18 months ago showed thickening of aryepiglottic fold and laryngeal mucosa reflecting chronic disease process. Autopsy showed chronic inflammation and lymphocytic infiltrate with atypical lymphocytes in all major organs including heart, lung, liver, kidney, brain, pancreas and upper airways and positive immunohistochemical staining for EBV (Fig. 1, 2).
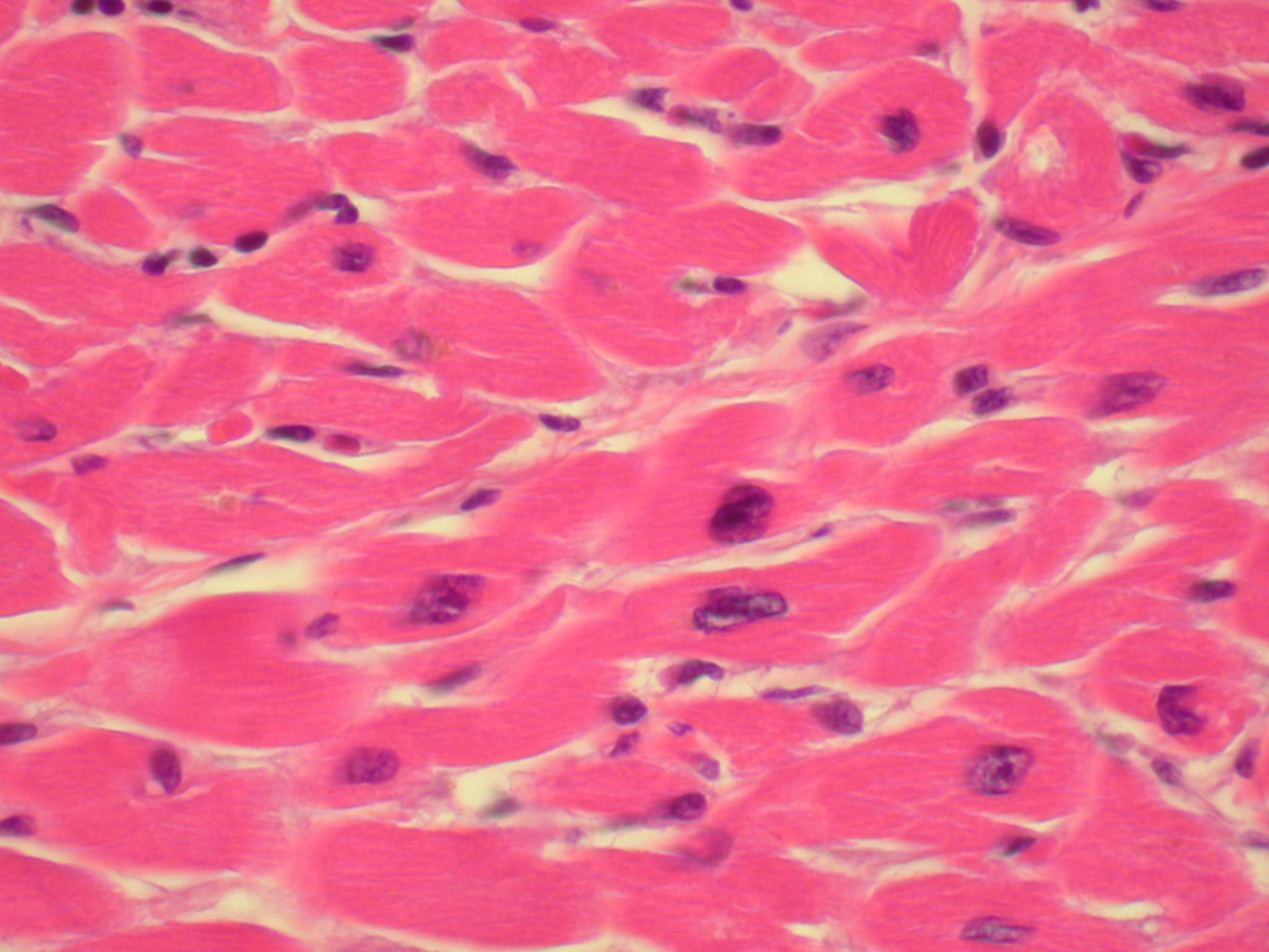 Click for large image | Figure 1. Diffuse myocyte hypertropy with atypical lymphocytes (× 40). |
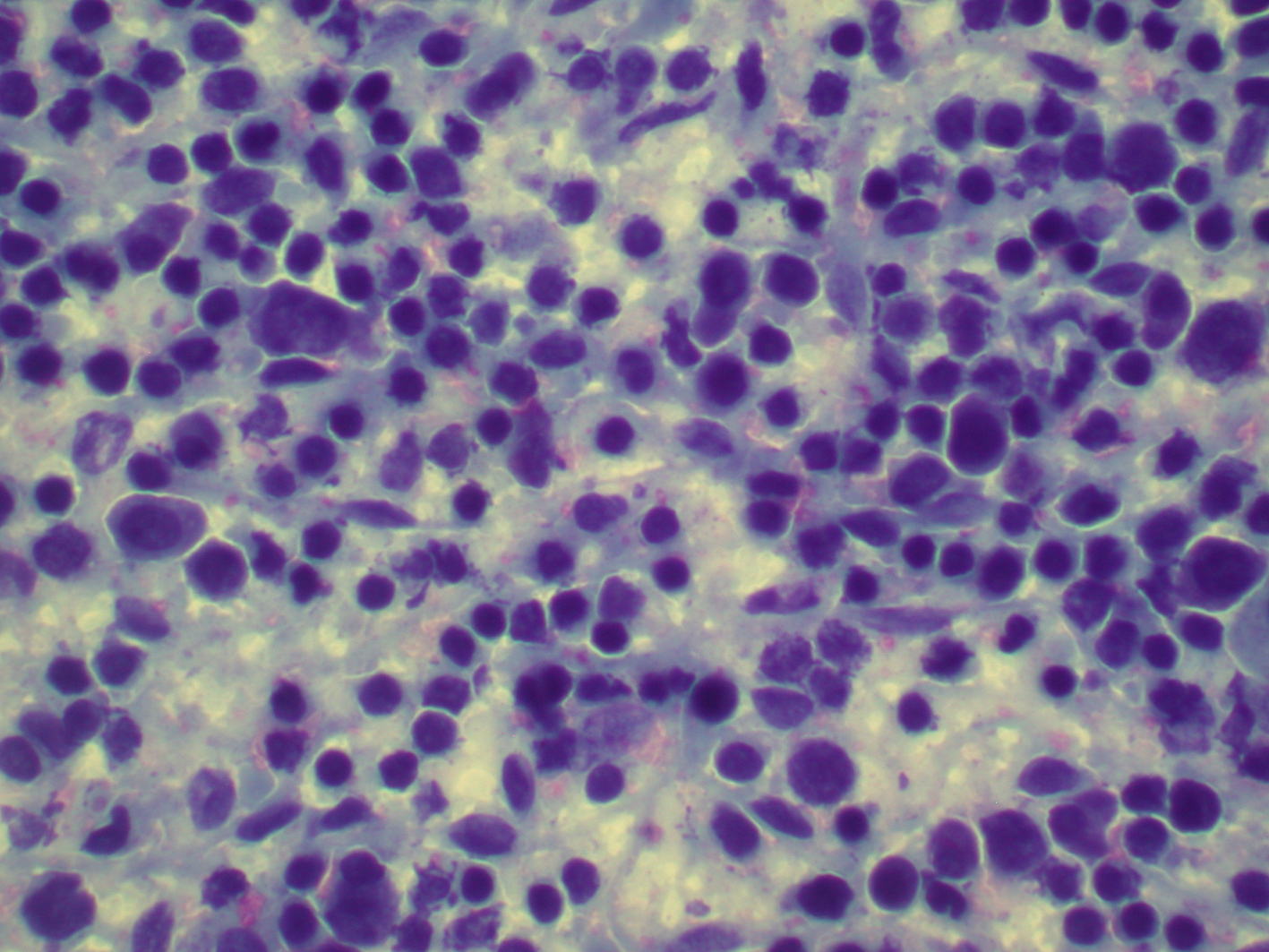 Click for large image | Figure 2. A large amount of atypical lymphocytes in spleen (× 40). |
| Discussion | ▴Top |
This seemingly immunocompetent young female had chronic progressive course of disease due to EBV which involved all major organs - a rare but fatal disease known as CAEBV infection with no known treatment currently available.
The disease has been defined by the presence of three features. 1) Severe progressive illness began as a primary EBV infection, or is associated with abnormal EBV-specific antibody titers. 2) Histology shows evidence of major organ involvement such as lymphadenitis, hemophagocytosis, meningoencephalitis or persistent hepatitis. 3) Elevated EBV DNA, RNA or proteins are demonstrable by in situ hybridization or immunohistochemical staining of affected tissues. Patients with CAEBV infection have unexplained illness lasting > 6 months and may have prolonged intermittent fever, continuous debilitating fatigue, sore throat, malaise, arthralgia, myalgia, or evidence of organ involvement like lymphadenopathy, hepatosplenomegaly, pneumonitis, uveitis, etc. [3, 4].
At least six specific EBV antibody tests help to determine the stage of EBV infection. These tests are expensive and not usually needed for the diagnosis of infectious mononucleosis. However, few serological characteristics may be helpful if CAEBV is suspected. Serological features that can be found in patients that can guide the diagnosis of CAEBV are as follows: 1) very high titers of EBV DNA in blood; 2) very high titers for antibodies (VCA-IgG > 1:640 and EA-IgG > 1:160); 3) once infected antibodies to EBNA persist for life, but patients with CAEBV infection may have absence of these antibodies; 4) IgA class antibodies against VCA and EA-D [5].
Majority of the patients with CAEBV suffer from an IM-like chronic illness. Some develop serious diseases such as EBV-related hemophagocytic lymphohistiocytosis or T-cell or NK-cell LPD/lymphomas during the course of illness. Many treatments including antiviral agents, immunomodulative therapy such as interferon gamma, IL-2, corticosteroids, cyclosporin A or immunoglobulins, and/or chemotherapeutic drugs have been tried without obvious effect on morbidity and outcome [6]. Not long ago, autologous EBV-CTL was given effectively in a series of patients with CAEBV [7]. Four of five patients did not show a relapse of their disease during the period of observation. Finally allogeneic bone marrow stem-cell transplantation or peripheral blood may be the treatment of choice as recently shown in the patients with severe disease [8].
Conclusion
CAEBV is a very rare life-threatening complication of EBV in healthy adults and can mimic various spectrum of clinical presentation and can mimic complications from different organ systems like diabetic ketoacidosis, ARDS, myocardial infarction, renal insufficiency, etc. and pose a great diagnostic challenge. A high index of clinical suspicion and certain unique serological features can help diagnose this very rare complication of EBV. Although there are reports of successful therapies with hematopoietic stem-cell transplants, the choice of therapy still remains a major therapeutic challenge. Underreporting of this very rare complication also adds to the lack of awareness to this rare and dreaded complication of CAEBV.
Grant Support
None.
| References | ▴Top |
- Longo DL, Harrison TR. Harrison's principles of internal medicine. New York: McGraw-Hill, Medical. 2012.
- Okano M, Matsumoto S, Osato T, Sakiyama Y, Thiele GM, Purtilo DT. Severe chronic active Epstein-Barr virus infection syndrome. Clin Microbiol Rev. 1991;4(1):129-135.
pubmed - Okano M. Features of Chronic Active Epstein-Barr virus Infection and Related Human Diseases. Open Hematology Journal. 2011;5.
- Sonke GS, Ludwig I, van Oosten H, Baars JW, Meijer E, Kater AP, de Jong D. Poor outcomes of chronic active Epstein-Barr virus infection and hemophagocytic lymphohistiocytosis in non-Japanese adult patients. Clin Infect Dis. 2008;47(1):105-108.
doi pubmed - Okano M, Kawa K, Kimura H, Yachie A, Wakiguchi H, Maeda A, Imai S, et al. Proposed guidelines for diagnosing chronic active Epstein-Barr virus infection. Am J Hematol. 2005;80(1):64-69.
doi pubmed - Okano M. Therapeutic approaches for severe Epstein-Barr virus infection. Pediatr Hematol Oncol. 1997;14(2):109-119.
doi pubmed - Savoldo B, Huls MH, Liu Z, Okamura T, Volk HD, Reinke P, Sabat R, et al. Autologous Epstein-Barr virus (EBV)-specific cytotoxic T cells for the treatment of persistent active EBV infection. Blood. 2002;100(12):4059-4066.
doi pubmed - Okamura T, Hatsukawa Y, Arai H, Inoue M, Kawa K. Blood stem-cell transplantation for chronic active Epstein-Barr virus with lymphoproliferation. Lancet. 2000;356(9225):223-224.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
