| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Case Report
Volume 2, Number 4-5, October 2012, pages 187-189
Acute Pancreatitis as the First Manifestation of Parathyroid Adenoma
Mehmet Akcea, e, Matthew Wascob, Beth Kimballc, Sima Saberid
aSaint Joseph Mercy Hospital, Department of Internal Medicine Ann Arbor, Michigan 48106, USA
bSaint Joseph Mercy Hospital, Department of Pathology, Ann Arbor, Michigan 48106, USA
cSaint Joseph Mercy Hospital, Department of General Surgery, Ann Arbor, Michigan 48106, USA
dAnn Arbor Endocrinology and Diabetes PC, Ypsilanti 48197, Michigan, USA
eCorresponding author: Mehmet Akce, Saint Joseph Mercy Hospital, Department of Internal Medicine Ann Arbor, Michigan 48106, USA
Manuscript accepted for publication August 17, 2012
Short title: Acute Pancreatitis
doi: https://doi.org/10.4021/jem114w
| Abstract | ▴Top |
Acute pancreatitis as a first manifestation of primary hyperparathyroidism (PHPT) caused by parathyroid adenoma is exceptionally rare. A 21 year old man presented with severe abdominal pain, nausea and vomiting. Laboratory studies revealed leukocytosis of 15.3 thousand/µL, hemoglobin 14.4 g/dL, creatinine 1.31 mg/dL, amylase 1,148 IU/L, lipase 862 IU/L. Serum calcium level was 14.6 mg/dL, intact parathyroid hormone (iPTH) level was 629.6 pg/mL. Neck ultrasound showed a 1.5 × 1 × 1.1 cm solid mass at the posterior inferior aspect of the right thyroid lobe. Parathyroid scan showed a focal area of activity in the right lower lobe suggesting a parathyroid adenoma. The patient underwent parathyroidectomy and pathological examination of the parathyroid gland confirmed a parathyroid adenoma. Although the actual causal relationship between hypercalcemia and pancreatitis has been a persistent topic of debate, detection of hypercalcemia may be a clue to diagnose PHPT due to parathyroid adenoma. After aggressive medical management of acute pancreatitis, parathyroidectomy may improve clinical outcome and prevent further recurrences of pancreatitis.
Keywords: Primary hyperparathyroidism; Acute pancreatitis
| Introduction | ▴Top |
Acute pancreatitis induced by hypercalcemia due to PHPT is a rare event and the reported incidence range from 0.23% to 6.8% [1, 2]. Acute pancreatitis as the first manifestation of PHPT caused by a parathyroid adenoma is exceptionally rare. The actual causal relationship between acute pancreatitis and PHPT has been a highly debated topic in the literature. Although there have been case series demonstrating a possible relationship between these two clinical entities [3, 4] population based studies have failed to show a true causal relationship between PHPT and acute pancreatitis [5, 6].
| Case Report | ▴Top |
A 21-year-old otherwise healthy man presented with sudden onset of abdominal pain, nausea, and vomiting. He was a smoker and consumed alcohol occasionally. He did not report any recent alcohol intake or medication use. On physical exam he had severe epigastric tenderness without rebound. Initial laboratory studies revealed leukocytosis of 15.3 thousand/µL, hemoglobin 14.4 g/dL, creatinine 1.31 mg/dL, amylase and lipase were elevated, 1,148 IU/L and 862 IU/L respectively. His ALT, AST, ALP, and total bilirubin were normal. Serum calcium level and albumin adjusted serum calcium level was significantly elevated, 14.6 mg/dL and 14.7 mg/dL respectively. Abdominal ultrasound revealed changes consistent with acute pancreatitis but no evidence of cholelithiasis, common bile duct dilation or sonographic evidence of acute cholecystitis. Given the absence of biliary-, alcohol- or medication associated pancreatitis, hypercalcemia was thought to be the potential culprit. Serum intact parathyroid hormone level was noted to be significantly elevated at 629.6 pg/mL (12 - 88 pg/mL), 25-hydroxy vitamin D level was 21 ng/mL. Neck ultrasound showed a 1.5 × 1 × 1.1 cm oval solid mass at the posterior inferior aspect of the right thyroid lobe (Fig. 1). A parathyroid scan showed a focal area of activity in the right lower lobe suggestive of a parathyroid adenoma (Fig. 2a, b). The patient was conservatively treated with IV fluids, pain medications, and he was given one dose of Pamidronate 60 mg. With these measures hisserum calcium decreased to 10.4 mg/dL. After his acute pancreatitis resolved he was discharged with scheduled elective parathyroidectomy as an outpatient. Two weeks later he was readmitted with nausea and vomiting. His serum calcium was 14.2 mg/dL with lipase 53 IU/L. After receiving IV fluids and Pamidronate, his serum calcium level decreased to 11.6 mg/dL. He underwent a parathyroidectomy during this second hospitalization and pathological examination revealed a 2.3 × 1.3 × 0.9 cm parathyroid adenoma (Fig. 3). His postoperative iPTH level was 1.2 pcg/mL and serum calcium level was 8.8 mg/dL, 25-hydroxy vitamin D level was 25 ng/mL. No further episodes of acute pancreaititis developed after the parathyroidectomy. One month after the parathyroidectomy his iPTH and calcium level were 91.2 pcg/mL and 7.7 mg/dL, respectively.
 Click for large image | Figure 1. Head and Neck Ultrasound showed 1.5 × 1× 1.1 cm oval solid mass at the posterior inferior aspect of the right thyroid lobe. |
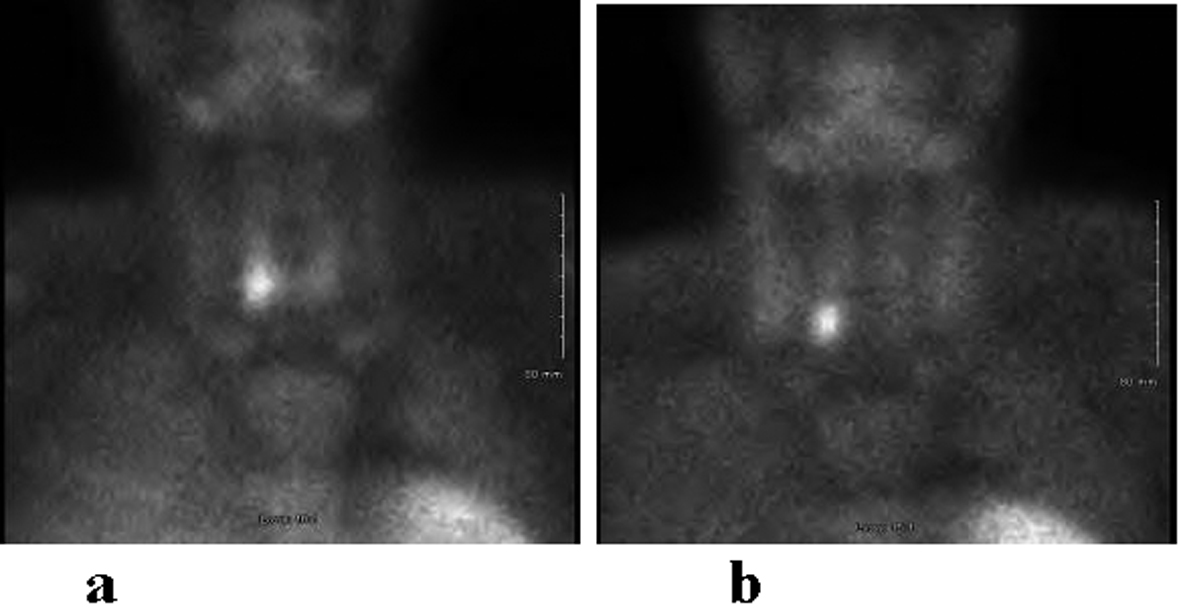 Click for large image | Figure 2. Following administration of 26.3 mCi 99m-technetium labeled Cardiolite, planar and SPECT images of the parathyroid gland were obtained. Immediate images (a) demonstrate a focal area of activity in the right lobe projected over the right lobe of the thyroid which persists on delayed image (b). Findings are consistent with parathyroid adenoma. |
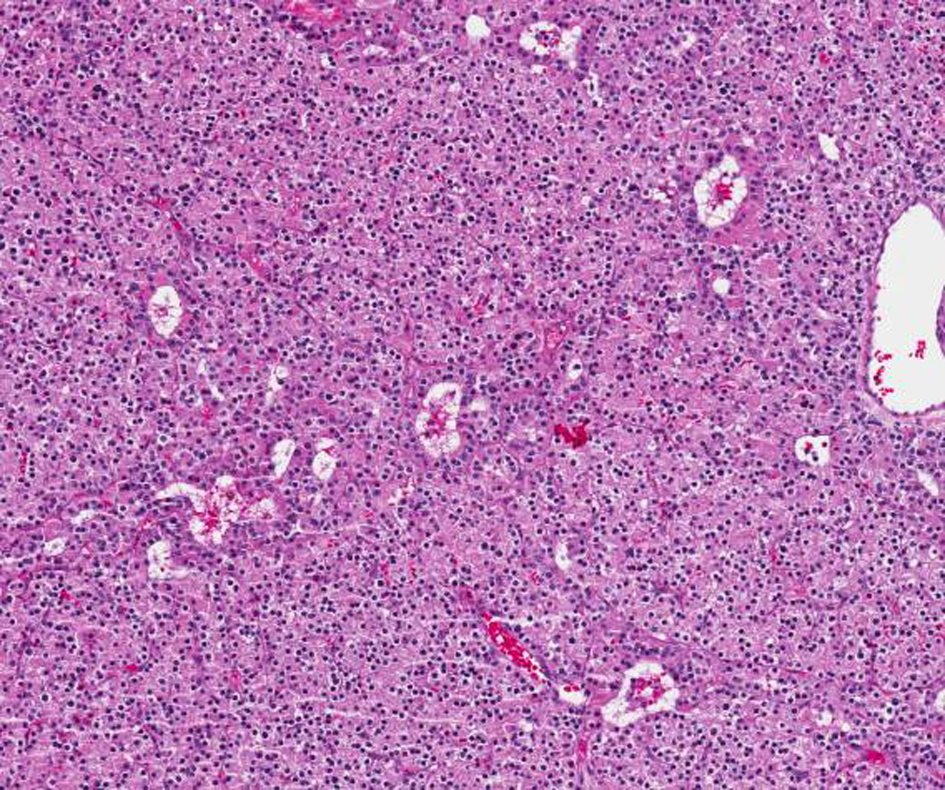 Click for large image | Figure 3. Hypercellular parathyroid gland consistent with adenoma. Nests of endocrine cells without significant atypia, occasional small cystic spaces and gland-like areas. |
| Discussion | ▴Top |
The incidence of acute pancreatitis in PHPT was found to be no different than in the general population in recent studies [5, 6] although the pancreatitis risk is known to be 10 fold elevated in PHPT [2]. Biliary stones and alcohol are responsible for 80% of acute pancreatitis cases whereas the remaining 20% can be related to various etiologies such as infection, ductal obstruction, hypercalcemia of any cause, hyperlipidemia, impaired pancreatic perfusion or idiopathic [1]. Hypercalcemia is one of the rare causes of acute pancreatitis and ectopic activation of trypsinogen to trypsin by hypercalcemia [7], hypercalcemia induced formation of pancreatic calculus [8] and genetic defects in SPINK 1 (serine protease inhibitor Kazal Type 1) and CFTR (cystic fibrosis transmembrane conductance regulator) genes [2] have been suggested as possible mechanisms of acute pancreatitis in the setting of hypercalcemia. Hypocalcemia is a poor prognostic factor in acute pancreatitis [9]. However, when hypercalcemia is detected in acute pancreaititis it should compel clinicians to search for alternative explanations such as malignancy or hyperparathyroidism. In this case the presence of hypercalcemia in acute pancreatitis guided us to detect undiagnosed PHPT and a parathyroid adenoma. Due to the patient’s unusually young age at the time of presentation, he was also screened for MEN-1 syndrome which was ruled out. The absence of any other explanation for acute pancreaititis and clinical improvement after parathyroidectomy supports a likely relationship between PHPT and acute pancreatitis in this case.
Conclusion
Although the actual causal relationship between hypercalcemia and pancreatitis has been a persistent topic of debate, detection of hypercalcemia may be a clue to diagnose PHPT due to parathyroid adenoma. After aggressive medical management of acute pancreatitis parathyroidectomy may improve clinical outcome and prevent further recurrences of pancreatitis.
| References | ▴Top |
- Sakorafas GH, Tsiotou AG. Etiology and pathogenesis of acute pancreatitis: current concepts. J Clin Gastroenterol. 2000;30(4):343-356.
doi - Felderbauer P, Karakas E, Fendrich V, Bulut K, Horn T, Lebert R, Holland-Letz T, et al. Pancreatitis risk in primary hyperparathyroidism: relation to mutations in the SPINK1 trypsin inhibitor (N34S) and the cystic fibrosis gene. Am J Gastroenterol. 2008;103(2):368-374.
doi pubmed - Carnaille B, Oudar C, Pattou F, Combemale F, Rocha J, Proye C. Pancreatitis and primary hyperparathyroidism: forty cases. Aust N Z J Surg. 1998;68(2):117-119.
doi pubmed - Jacob JJ, John M, Thomas N, Chacko A, Cherian R, Selvan B, Nair A, et al. Does hyperparathyroidism cause pancreatitis? A South Indian experience and a review of published work. ANZ J Surg. 2006;76(8):740-744.
doi pubmed - Khoo TK, Vege SS, Abu-Lebdeh HS, Ryu E, Nadeem S, Wermers RA. Acute pancreatitis in primary hyperparathyroidism: a population-based study. J Clin Endocrinol Metab. 2009;94(6):2115-2118.
doi pubmed - Bess MA, Edis AJ, van Heerden JA. Hyperparathyroidism and pancreatitis. Chance or a causal association? JAMA. 1980;243(3):246-247.
doi pubmed - Frick TW, Fernandez-del Castillo C, Bimmler D, Warshaw AL. Elevated calcium and activation of trypsinogen in rat pancreatic acini. Gut. 1997;41(3):339-343.
doi pubmed - Cope O, Culver PJ, Mixter CG, Jr., Nardi GL. Pancreatitis, a diagnostic clue to hyperparathyroidism. Ann Surg. 1957;145(6):857-863.
doi pubmed - Ranson JH. Etiological and prognostic factors in human acute pancreatitis: a review. Am J Gastroenterol. 1982;77(9):633-638.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
