| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Review
Volume 13, Number 2, June 2023, pages 43-48
Approach to the Patient With Pituitary Adenoma Using Telemedicine: Knowledge Gaps and Recommendations
Abdulhameed Alhazmia, e, f , Wael Almistehib, Moeber Mahzaric, d, e
aInternal Medicine Department, Jazan University Hospital, Jazan University, Jazan, Saudi Arabia
bObesity, Endocrine, and Metabolism Center, King Fahad Medical City, Riyadh, Saudi Arabia
cCollege of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
dKing Abdullah International Medical Research Center, Riyadh, Saudi Arabia
eDepartment of Medicine, Ministry of the National Guard-Health Affairs, Riyadh, Saudi Arabia
fCorresponding Author: Abdulhameed Alhazmi, Internal Medicine Department, Jazan University Hospital, Jazan University, Jazan, Saudi Arabia
Manuscript submitted February 7, 2023, accepted March 18, 2023, published online April 30, 2023
Short title: Patient With Pituitary Adenoma Using TM
doi: https://doi.org/10.14740/jem866
- Abstract
- Introduction
- Search Strategies
- Current Knowledge
- Evaluation of Pituitary Adenoma Patients With TM
- Obtaining Virtual History
- Performing Virtual Physical Examination
- Virtual Laboratory and Imaging Investigations
- Virtual Management and Follow-Up
- Future of TM Use in the Care of Pituitary Adenoma
- Conclusion
- References
| Abstract | ▴Top |
Telemedicine (TM) can be defined as the practice of medicine using technology such as video teleconferencing, telephone calls, or emails in order to provide health care from a distance. The emergence of the coronavirus disease 2019 (COVID-19) pandemic and its potential complications have created an urgent need for the transformation of physical visits into virtual encounters. Pituitary adenomas are one of the common endocrine tumors and can manifest with hormonal or mass effects. COVID-19 impacted the common pathway of diagnosis and treatment of these masses. TM utilization for pituitary adenomas has not been addressed thoroughly in the literature despite how common they are. In this review article, we discuss and implement what has been written in the literature about TM for pituitary adenoma alongside our suggested protocol.
Keywords: Telemedicine; Pituitary adenoma; Telehealth; Pituitary disorders
| Introduction | ▴Top |
The pituitary gland controls the regulation of most endocrine glands; therefore, it is referred to as the “master gland”. It occupies the sella turcica, inferior to the optic chiasm, and secretes the luteinizing hormone, follicle-stimulating hormone, adrenocorticotropic hormone, prolactin, the thyroid-stimulating hormone, and the growth hormone and stores oxytocin and the antidiuretic hormone, which are produced by the hypothalamus. Pituitary adenomas are considered one of the most common sella tumors. They can manifest with hyper or hypofunction, and the mass effect causing pressure to the surrounding structures. Alternatively, they can be asymptomatic and can be found as incidental masses in imaging studies [1]. A pituitary adenoma is usually classified based on the tumor’s longest diameter into microadenoma (< 1 cm) or macroadenoma (≥ 1 cm). Further categorization considers the cell of origin, which can be a hormone-producing or non-functional adenoma [2]. The prolactin-secreting pituitary adenoma, growth hormone-secreting adenoma, and non-functional pituitary adenoma are the most common causes of pituitary masses [2]. Worldwide prevalence of pituitary adenomas has been estimated to be around 76 to 116 cases per 100,000 population [3, 4]. The prevalence varies depending on the geographic locations. For example, in Iceland, Agustsson et al reported a prevalence of 1 in 865 individuals [5]. On the other hand, Tjornstrand et al reported pituitary adenoma prevalence of 1 in 2,688 individuals in Sweden [6]. Moreover, the incidence of new cases of pituitary adenomas has been increasing and is estimated to be around 5.1/100,000 per year [4].
The management of such cases and follow-up plans vary depending on the tumor characteristics, which include symptoms, the size of the mass, and the type of the originating cells [2].
Telemedicine (TM) has been proven safe and effective in multiple aspects of endocrinological disorders, including preoperative management of pheochromocytoma and thyrotoxicosis treatment [7, 8]. Recently, the emergence of the coronavirus disease 2019 (COVID-19) pandemic and its potential complications gave rise to safety concerns among patients regarding face-to-face encounters with medical healthcare providers, particularly with inpatient service [9]. Anxiety and the fear of getting infected with COVID-19 may influence patients’ compliance with appointments, leading to significant adverse sequelae. As such, the utilization of TM services has increased expediently since the pandemic. Addressing pituitary adenoma management via TM has been implemented for different reasons, including long distances, neuropsychological difficulties, and COVID-19 precautions [10-13].
TM has shown a significant impact on patients’ lives and economic settings. It helped patients with physical difficulties or in rural areas without access to a specialized care, where a delay in pituitary adenoma management can lead to some serious complications including: pituitary apoplexy, electrolytes disturbance and cardiac morbidity [11]. In addition, a cost reduction was observed compared to face-to-face encounters [12, 14, 15]. This article reviews the literature regarding the implementation of TM for pituitary adenoma patients alongside our suggested protocol. It is beyond the scope of this review to discuss pituitary adenoma management in detail, as this is published elsewhere.
| Search Strategies | ▴Top |
Papers written in English and published from April 2000 until April 2022 and available in Google Scholar and PubMed databases were collected and examined.
Adults whom are 18 years or above were included, and those who are below were omitted from the study. Only four articles were found: two case reports, one original research, and one poster.
| Current Knowledge | ▴Top |
Different articles in the literature described the utilization of TM for prolactinoma, non-functional pituitary adenoma, and acromegaly [10-13]. However, the reasons behind these studies varied. For example, Hiba et al’s reported a case in which a patient was diagnosed with macroadenoma secondary to prolactinoma and managed with a face-to-face encounter. Once the patient became stable, and the far distance of his home was taken into account, they shifted him to TM follow-ups [10]. On the other hand, Zahid et al reported a case that showed a need for endocrine expert opinion. They described a patient from Nigeria presented with hypopituitarism and visual symptoms, and his physician asked for an overseas consultation, which revealed a non-functional macroadenoma after evaluation. The patient had transsphenoidal surgery in the United Kingdom, and then traveled back to Nigeria, where he continued to follow up with the United Kingdom endocrinologists through TM [11]. Naves et al aimed to implement a TM protocol for acromegaly patients to provide social distancing and decrease the risk of exposure to COVID-19 infection [12]. The patient satisfaction was initially high, but it subsided after 6 months, suggesting that there is a need for face-to-face encounters for long-term follow-ups. It is yet early to judge Guilia et al’s poster since their current data are preliminary. However, it looks promising from results suggestive of an increase in patients’ compliance with medications [13].
| Evaluation of Pituitary Adenoma Patients With TM | ▴Top |
The endocrine specialist is usually the second or third physician that a patient is referred to, depending on how the first medical service evaluates the patient. It is essential to have a history, physical examination, diagnostics results, and management plan that have been compiled in a clear, detailed referral form, especially when an endocrinologist is going to see the patient virtually for the first time. Selecting a suitable patient enrolled in the TM pathway can be challenging. We can classify the factors affecting the selection of a patient into three classes: legal, patient-related, and technical. Considering the opportunity to perform a comprehensive assessment with a detailed physical examination, we recommend that the first two visits be face-to-face, followed by TM [16]. However, evaluating patients using TM for the first time is possible, especially in the absence of a specialist endocrine center nearby. Table 1 summarizes the factors that should exclude the patient from being seen virtually [10, 12].
 Click to view | Table 1. Exclusion Criteria for the Implementation of TM With Pituitary Adenoma Patients |
| Obtaining Virtual History | ▴Top |
Depending on the cause of the pituitary tumor, taking the patient’s history during the tele-encounter is no different from that of the face-to-face encounter. The physician should give significant attention to symptoms suggestive of mass effect, including visual impairment, headaches, altered levels of consciousness, nausea, and vomiting. In addition, he or she must obtain a history of pituitary hormone hypersecretion or hyposecretion symptoms. However, there are some aspects that need to be kept in mind during TM encounters. Technical issues can present at any time during the encounter; thus, it is crucial to pay attention to some details more than others to maximize the benefits of the encounter. To facilitate the virtual encounter, we recommend that before starting the encounter, the physician reviews the patient’s file, determines the format of the visit (audio only or video), and writes down the most critical questions that need to be asked of the patient. Once the virtual encounter has started, the physician must present himself, confirm the patient’s identity and attain verbal consent. It is essential to assess audio or video quality with confirmation that the other party can hear and see the physician. Looking directly at the camera will ensure eye contact with the patient. Before obtaining the patient history, explain to the patient the privacy of the call, emphasizing that the encounter is not being recorded.
| Performing Virtual Physical Examination | ▴Top |
Physical assessment is a dilemma with virtual care [16]. There is no palpation, percussion, or auscultation, only inspection. When it comes to pituitary adenomas, the examination should begin directly from the start of the encounter. If the encounter is telephone-based (audio only), and there is a need for physical examination, the physician can ask the patient to switch to a video call. If it is a video call, attention should be given to the patient’s general condition: anxiety, sweating, and mental status. The patient can take their own vital signs with the appropriate equipment if it is available, such as a thermometer, digital sphygmomanometer, glucometer, and smartwatch that monitors pulse rate and oxygen saturation. Supposing the patient agrees, a companion can assist in performing clinical examination maneuvers, like checking for orthostatic hypotension with the help of the physician’s instructions. One significant pituitary adenoma sequela is visual impairment, representing up to 60% of related symptomatic mass effects. A referral for an ophthalmologist to conduct an appropriate assessment is warranted in the presence of visual defects. Despite the advances in ophthalmology TM, it still lacks comprehensive evaluation [17]. Usually, the health care provider can observe facial features of acromegaly and Cushing’s disease, and if the TM platform allows data sharing, the patient can share an old photo to compare. Other features of Cushing’s disease, such as abdominal striae or hand features of acromegaly, can be visually identified through the camera. However, examination of breast enlargement, nipple discharge, or testicular size may cause some embarrassment or lead to unpleasant feelings, so we advise avoiding obtaining them until further updated research studies.
| Virtual Laboratory and Imaging Investigations | ▴Top |
Laboratory evaluation takes the same approach. If hypersecretion is the concern, the physician will require the patient to do the following tests: early morning blood cortisol, thyroid-stimulating hormone, free T4, prolactin, insulin-like growth factor-1 (IGF-1), total testosterone in men/estrogen in women, and screening tests for Cushing’s disease if there is clinical suspicion of such. When hypopituitarism is the concerned disorder, the addition of the adrenocorticotropic hormone and synacthen test is needed for a better evaluation [18, 19]. According to the diagnosis and treatment plan, imaging modalities with head computed tomography (CT) or pituitary magnetic resonance imaging (MRI) with contrast should follow. The utilization of diagnostic modalities with TM is a straightforward case compared to history taking and physical examination. The patient can do the laboratory or imaging studies in an affiliated center. Then, either the patient or the referring physician will relay the laboratory results to the endocrinologist to complete the assessment in what is known as asynchronous TM.
| Virtual Management and Follow-Up | ▴Top |
The maintenance treatment goals for pituitary tumors are: 1) Reduction of hormonal hypersecretion and its clinical sequelae; 2) Shrinkage of tumor size to decrease mass effect symptoms; 3) Replacement of deficient hormones.
Most pituitary adenomas are managed by surgical excision via a transsphenoidal approach, especially when there is a mass effect [20]. However, medical therapy with dopamine agonists such as cabergoline is preferred for prolactinoma [21]. When patients have hypopituitarism, treatment focuses on replenishing deficient hormones and emphasizes steroids and thyroid hormone replacement.
The complexity of the tumor management may require a multidisciplinary meeting, especially when surgery is needed. TM implementation in multidisciplinary meetings has improved the access and collaboration of medical experts, enhancing medical competence, delivery of diagnosis, and treatment alongside follow-up [22]. The physician or the coordinator can hold a video teleconference involving an endocrinologist, ophthalmologist, and neurosurgeon to discuss the most appropriate treatment plan for the patient. A further meeting can be arranged based on individual needs. For instance, a video teleconference with a cardiology or gastroenterology service to discuss acromegaly complications. Multidisciplinary video teleconferencing may be used for educational purposes as well. The patient can be invited to join the meeting and listen to every specialized part of the management plan, thus reducing the need for multiple future appointments. Table 2 highlights the essential aspects of TM virtual encounters with a pituitary adenoma patient.
 Click to view | Table 2. Aspects of a Virtual Encounter With a Pituitary Adenoma Patient |
TM is a great practice that can save costs and reduce waiting time. However, it is not without downsides. As a starter, the laws differ from country to country regarding the organizing authority, which digital applications the physician or health care provider can use, data privacy, and insurance coverage [11]. Another explicit limitation is the lack of appropriate application of physical examination, which made some physicians reluctant to use it [12, 16]. One last point to take into consideration is that the longer the duration of a virtual encounter, the more a face-to-face visit is needed to keep up with the patient [12]. Our suggestive protocol for pituitary adenoma enrollment is shown in Figure 1.
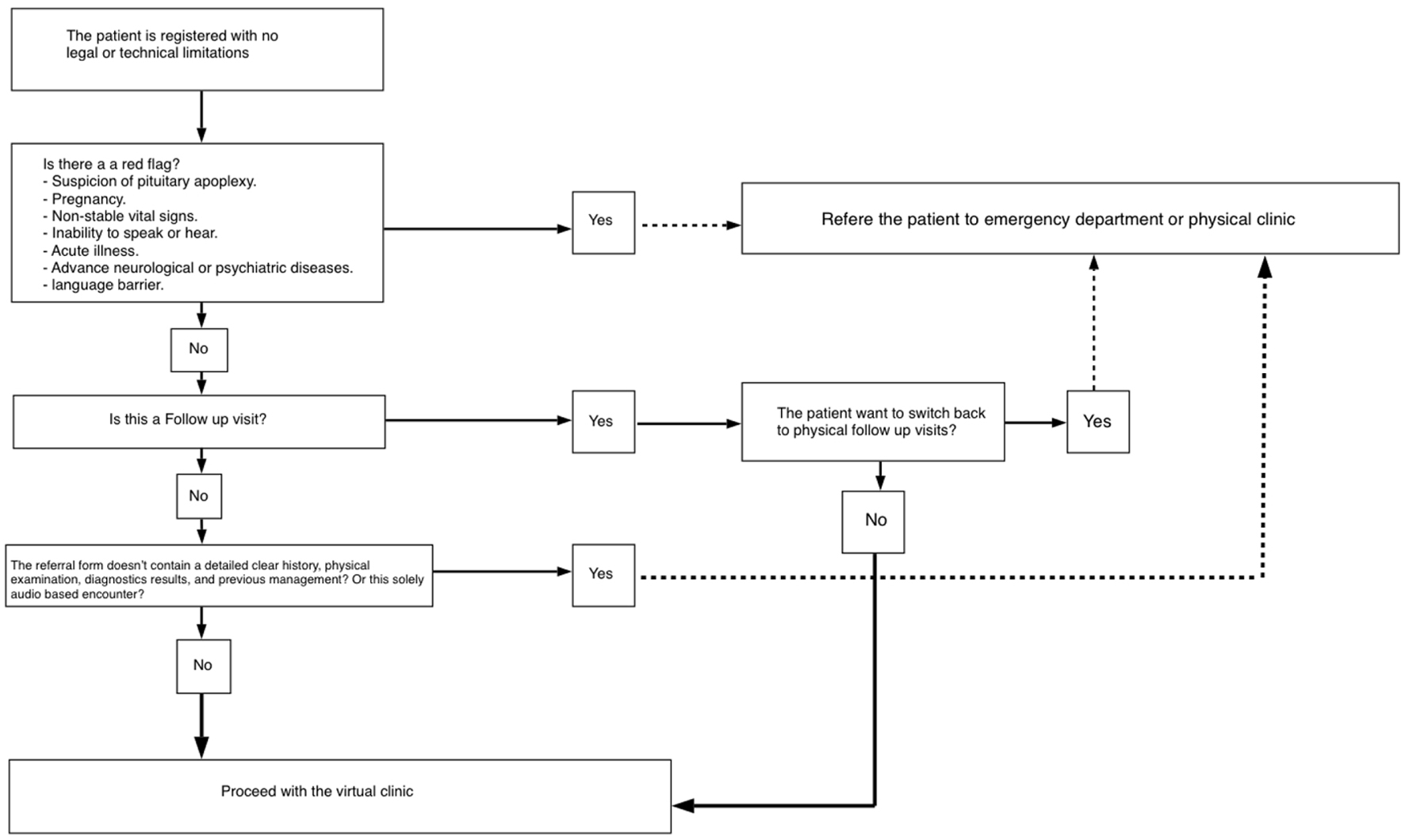 Click for large image | Figure 1. Protocol for pituitary adenoma patient’s enrollment in TM. Initially, there should be no legal or technical aspects prohibiting a proper TM encounter. After that, if the patient exhibits any red flags or has technical difficulties, the physician should refer him/her to an emergency service or physical encounter. The following steps depend on visit status: first or follow-up visit. If it is a first visit, an adequately documented history, physical examination, and follow-up should be available before proceeding with the TM encounter. Without proper documentation, we suggest switching the patient to a physical clinic for the first visit. To ensure patient satisfaction, if the patient is a chronic patient with a previous TM, it is valuable to give the patient the option to choose between physical or the TM encounter before proceeding with the encounter. TM: telemedicine. |
| Future of TM Use in the Care of Pituitary Adenoma | ▴Top |
The benefits of TM in healthcare became evident during COVID-19, and its use beyond this era is appealing. TM improves timely healthcare access and reduces healthcare costs. Establishing adequate TM infrastructures is key in expanding TM’s role in healthcare. Moreover, developing regulations for TM use in terms of licensing its use and the type of care provided via TM is needed [23].
Guidelines on the use of TM in pituitary adenomas are limited and depend on the legal system, the availability of the infrastructure, and expert clinical judgment. For example, Khalil et al utilized TM in the aspect of follow-up, whereas Khan et al applied it to the physician-to-physician consult and in the term of follow-up as well [10, 11]. Guidelines on the use of TM in pituitary adenomas are limited and depend on the legal system, the availability of the infrastructure, and expert clinical judgment. For example, Khalil et al utilized TM in the aspect of follow-up, whereas Khan et al applied it to the physician-to-physician consult and in the term of follow-up as well [10, 11]. Despite the current suggested policies and general statements about the application of TM in endocrinology, further studies are concerned to establish a clear TM protocol for pituitary adenoma [24].
| Conclusion | ▴Top |
This article demonstrates how the pituitary disorders in form of adenomas may benefit from the various advantages of TM, such as reduced costs, decreased waiting time, and access to endocrine specialists from rural areas. However, challenges lie in the differences in international legal aspects and the limitation of physical examinations. We encourage a further study on the implementation of TM for pituitary disorders since it will significantly impact global advances in endocrinology.
Acknowledgments
None to declare.
Financial Disclosure
The authors did not receive support from any organization for the submitted work.
Conflict of Interest
The authors declare there are no conflict of interest.
Author Contributions
All authors have contributed in writing, editing, and reviewing the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Famini P, Maya MM, Melmed S. Pituitary magnetic resonance imaging for sellar and parasellar masses: ten-year experience in 2598 patients. J Clin Endocrinol Metab. 2011;96(6):1633-1641.
doi pubmed pmc - Molitch ME. Diagnosis and treatment of pituitary adenomas: a review. JAMA. 2017;317(5):516-524.
doi - Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML, McCutcheon IE. The prevalence of pituitary adenomas: a systematic review. Cancer. 2004;101(3):613-619.
doi - Daly AF, Beckers A. The epidemiology of pituitary adenomas. Endocrinol Metab Clin North Am. 2020;49(3):347-355.
doi - Agustsson TT, Baldvinsdottir T, Jonasson JG, Olafsdottir E, Steinthorsdottir V, Sigurdsson G, Thorsson AV, et al. The epidemiology of pituitary adenomas in Iceland, 1955-2012: a nationwide population-based study. Eur J Endocrinol. 2015;173(5):655-664.
doi - Tjornstrand A, Gunnarsson K, Evert M, Holmberg E, Ragnarsson O, Rosen T, Filipsson Nystrom H. The incidence rate of pituitary adenomas in western Sweden for the period 2001-2011. Eur J Endocrinol. 2014;171(4):519-526.
doi - Heslin MJ, Liles JS, Moctezuma-Velazquez P. The use of telemedicine in the preoperative management of pheochromocytoma saves resources. Mhealth. 2019;5:27.
doi pubmed pmc - Griffith ML, Bischoff LA, Baum HBA. Approach to the patient with thyrotoxicosis using telemedicine. J Clin Endocrinol Metab. 2020;105(8):2812-2818.
doi pubmed pmc - Fleseriu M, Dekkers OM, Karavitaki N. Endocrinology in the time of COVID-19: Management of pituitary tumours. Eur J Endocrinol. 2020;183(1):G17-G23.
doi pubmed pmc - Khalil H, Abdelnabi R, Osman A, Bashari WA. Applying telemedicine technology in treating prolactinomas: a case report. Cureus. 2020;12(7):e9043.
doi pubmed pmc - Khan Z, Mlawa G, Yousif Y, Afghan A, Balami D, Mohammed M, Muhammad S, et al. The future of cross-continental telemedicine in the management of complicated endocrine patients and its suitability based on a case report. Cureus. 2022;14(2):e22174.
doi pubmed pmc - Naves LA, Rosa IN, Lima TAS, Santana LB, Castro LF, Casulari LA. Implementation and monitoring of a telemedicine model in acromegalic outpatients in a low-income country during the COVID-19 pandemic. Telemed J E Health. 2021;27(8):905-914.
doi - Del Sindaco G, Sala E, Carosi G, Verrua E, Serban AL, Ferrante E, Mantovani G. Telemedicine in the management of acromegalic patients. Endocrine Abstracts. Bioscientifica. 2019;63:P1006.
- Karimi M, Lee EC, Couture SJ, Gonzales AB, Grigorescu V, Smith SR, De Lew N, et al. National trends in telehealth use in 2021: disparities in utilization and audio vs. video services. (Research Report No. HP-2022-04). Office of the Assistant Secretary for Planning and Evaluation, U. S. Department of Health and Human Services. February 2022.
- Kichloo A, Albosta M, Dettloff K, Wani F, El-Amir Z, Singh J, Aljadah M, et al. Telemedicine, the current COVID-19 pandemic and the future: a narrative review and perspectives moving forward in the USA. Fam Med Community Health. 2020;8(3):e000530.
doi pubmed pmc - Jin MX, Kim SY, Miller LJ, Behari G, Correa R. Telemedicine: current impact on the future. Cureus. 2020;12(8):e9891.
doi pubmed pmc - Conway J, Krieger P, Hasanaj L, Sun L, Scharf JM, Odel JG, Dinkin MJ, et al. Telemedicine evaluations in neuro-ophthalmology during the COVID-19 pandemic: patient and physician surveys. J Neuroophthalmol. 2021;41(3):356-361.
doi - Melmed S. Pituitary-tumour endocrinopathies. New England Journal of Medicine. 2020;382:937-950.
doi - Fleseriu M, Hashim IA, Karavitaki N, Melmed S, Murad MH, Salvatori R, Samuels MH. Hormonal replacement in hypopituitarism in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(11):3888-3921.
doi - Lithgow K, Batra R, Matthews T, Karavitaki N. Management of endocrine disease: visual morbidity in patients with pituitary adenoma. Eur J Endocrinol. 2019;181(5):R185-R197.
doi - Varlamov EV, McCartney S, Fleseriu M. Functioning pituitary adenomas - current treatment options and emerging medical therapies. Eur Endocrinol. 2019;15(1):30-40.
doi pubmed pmc - Aghdam MRF, Vodovnik A, Hameed RA. Role of telemedicine in multidisciplinary team meetings. J Pathol Inform. 2019;10:35.
doi pubmed pmc - Bhaskar S, Nurtazina A, Mittoo S, Banach M, Weissert R. Editorial: telemedicine during and beyond COVID-19. Front Public Health. 2021;9:662617.
doi pubmed pmc - Vimalananda VG, Brito JP, Eiland LA, Lal RA, Maraka S, McDonnell ME, Narla RR, et al. Appropriate use of telehealth visits in endocrinology: policy perspective of the endocrine society. J Clin Endocrinol Metab. 2022;107(11):2953-2962.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
