| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Case Report
Volume 13, Number 1, February 2023, pages 39-42
Sheehan’s Syndrome in a Fifty-Six-Year-Old Woman Presenting With a Retroperitoneal Mass: Perioperative Management During a Major Surgery
Department of Clinical Science, College of Medicine, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Manuscript submitted January 1, 2023, accepted February 7, 2023, published online February 17, 2023
Short title: Perioperative Management of Sheehan’s Syndrome
doi: https://doi.org/10.14740/jem858
| Abstract | ▴Top |
Patients with Sheehan’s syndrome (SS) can present with adrenal crisis, myxedema coma, hypoglycemia, and hyponatremia, which could be triggered by an infection or surgery. For the endocrinologist, a patient with SS who is scheduled for surgery presents a significant challenge as more likely to experience delayed emergence from anesthesia, hypotension that does not respond to the standard regimen, a decrease in core body temperature, and a decreased need for anesthetic drugs due to reduced metabolism. Here, to emphasize the significance of perioperative management to reduce the risk of morbidity and mortality from a potential adrenal crisis, we report the successful perioperative management of a 56-year-old woman with SS undergoing major surgery for the resection of a retroperitoneal tumor. The management plan for this patient comprised a perioperative intravenous hydrocortisone supplementation and thyroxine tablets on the morning of the procedure. In the operating room, the patient was started on norepinephrine, and she was given intravenous (IV) crystalloids and albumin. Healthcare providers should be aware of the perioperative risk of SS. No consensus, guidelines, or randomized trials for the safe perioperative management of patients with SS have been identified by a thorough review of the literature. Because of this, the perioperative care of these patients necessitates the utmost caution in addition to successful management based on close coordination between the endocrinologist, surgeon, and anesthetist.
Keywords: Sheehan syndrome; Adrenal insufficiency; Hypopituitarism; Perioperative management
| Introduction | ▴Top |
Sheehan’s syndrome (SS) is primarily caused by ischemic pituitary necrosis due to hemorrhage related to childbirth that results in reduced perfusion of the pituitary [1, 2]. Patients with SS frequently experience secondary hypothyroidism and adrenal insufficiency [3]. SS can occasionally present as an emergency with circulatory collapse, severe hyponatremia, and hypoglycemia. These symptoms may be brought on by an infection or surgery [4]. Here, we report the successful perioperative management of a 56-year-old woman with SS undergoing major surgery for the resection of a retroperitoneal tumor to emphasize the significance of perioperative management to reduce the risk of morbidity and mortality from a potential adrenal crisis.
| Case Report | ▴Top |
Investigations
Our patient is a 56-year-old woman known to have SS for 25 years diagnosed after postpartum hemorrhage following the delivery of her third child. She undergoes follow-up at the endocrinology clinic, and she is currently on levothyroxine 100 µg daily and prednisone 5 mg every other day. She is also known to have had type-2 diabetes, hypertension, and dyslipidemia in the past 14 years, and she is undergoing follow-up at her local hospital with appropriate control.
Diagnosis
The patient was referred from her local hospital complaining of right lower quadrant and periumbilical pain for the last 6 months that was intermittent. On physical examination, she appeared conscious and cooperative, and her vital signs were stable. Abdomen was soft and lax with no hepatosplenomegaly, and the mass was felt in the right lower quadrant. Examination of other systems was unremarkable. Computed tomography (CT) findings suggested a right posterior abdominal wall/retroperitoneal infiltrative mass measuring 88 × 68 × 67 mm. The possible differential was hemangioma, lipoma, liposarcoma, or angiomyolipoma that could not be entirely excluded radiologically. The patient was admitted for investigation and possible intervention. Magnetic resonance imaging (MRI) revealed an ill-defined right retroperitoneal vascular lesion just cranial to the right iliac crest, likely to represent an arteriovenous (AV) malformation with surrounding desmoplastic reaction.
Her laboratory findings and hormonal profile are shown in Table 1. MRI shows the pituitary gland compressed in the floor of the sella turcica suggesting an empty sella (Fig.1).
 Click to view | Table 1. Hormonal Profile of the Anterior Pituitary |
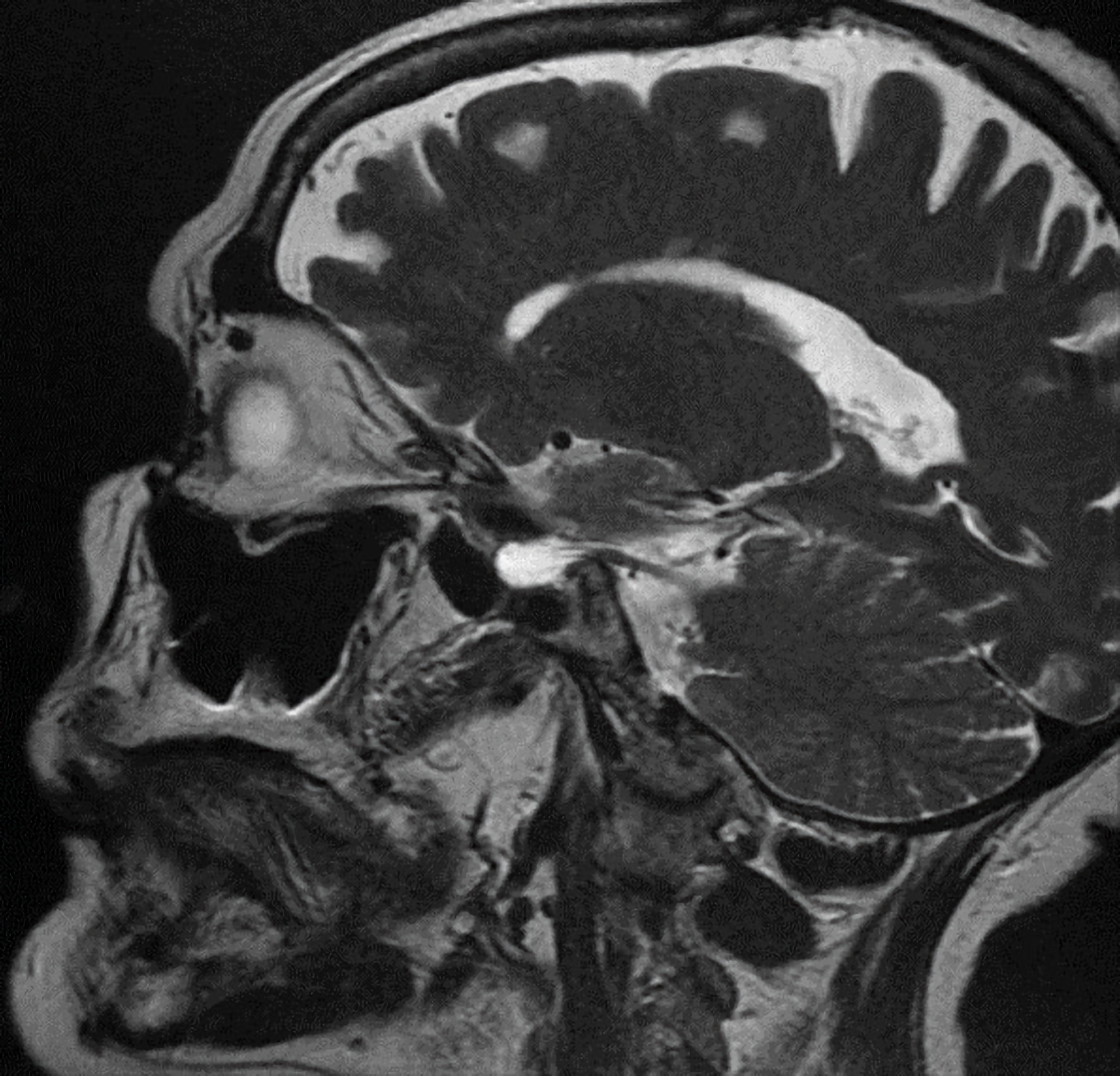 Click for large image | Figure 1. Sagittal view of pituitary MRI showing pituitary fossa filled with cerebrospinal (empty sella). MRI: magnetic resonance imaging. |
This work has been approved by the PNU Institutional Review Board (IRB) with IRB log number 22-1130.
Treatment
The patient went for elective surgery for resection of the retroperitoneal mass. The main concern was the difficult surgery due to the highly vascular mass with big size that was infiltrating the retroperitoneum. So, the perioperative adjustment of medications was crucial to avoid crisis. A multidisciplinary team with endocrinologists, surgeons, and anesthesiologists worked together.
She was scheduled for perioperative intravenous hydrocortisone supplementation. She was instructed to refrain from eating or drinking for 8 h prior to the procedure and to take a thyroxine tablet with sips of water the morning of the procedure. In the operating room, the patient was hypotensive on induction, so she was started on norepinephrine 0.1 µg/kg/min, the dose was increased until 0.7 µg/kg/min as the max dose and was kept on 0.7 µg/kg/min when she was sent to the intensive care unit (ICU). Two liters of crystalloids and 500 mL of 5% albumin were given. During surgery, which lasted 100 min, blood glucose was 19 mmol/L, so insulin infusion was initiated and replacing potassium accordingly. The estimated blood loss during surgery was 700 mL. A stress dose of 100 mg intravenous injection of hydrocortisone in two divided doses separated by 3 h were given, at the induction of anesthesia, followed by a 4 mg/h infusion until oral intake was resumed after surgery; then the patient was given hydrocortisone 50 mg, oral, three times a day (TID) for 2 days, then she was shifted to 5 mg prednisone orally daily.
Follow-up and outcomes
The patient suffered from hyponatremia (Na = 130 on day 3 postoperative) and gradually improved onwards spontaneously. The patient responded well to hormonal replacement therapy and intravenous rehydration. Her blood pressure, electrolytes, and blood sugar levels were normal during her postoperative stay. Pathology report revealed a retroperitoneal AV malformation.
| Discussion | ▴Top |
Patients with SS can present with adrenal crisis, hypoglycemia, and hyponatremia, which could be triggered by an infection or surgery [4]. As a result of hypopituitarism, the mortality rate of patients with SS is 1.2 to 2.17 times higher than that of the general population [5]. For the endocrinologist, the anesthetist and the surgical team, a patient with SS who is scheduled for surgery presents a significant challenge. A patient with SS is more likely to experience postoperative gastrointestinal and neuropsychiatric complications, electrolyte and coagulation disturbances, delayed emergence from anesthesia, perioperative stress management, and steroid management. The anesthetic complications in a patient with SS also include hypotension that does not respond to the standard regimen, a decrease in core body temperature, and a decreased need for anesthetic drugs due to reduced metabolism [6]. In our patient, the surgery was planned with a lower anesthetic dose in light of all these concerns. Due to multiple endocrinological problems and the presence of the retroperitoneal mass, our patient was posted for elective resection of the mass. Anemia, hypotension, and postpartum hemorrhage are the three main factors that predispose to adrenal crisis in women with SS, according to a thorough literature review by Matsuzaki et al [6]. During surgery, our patient’s blood pressure dropped and was corrected by stress dose of steroids, norepinephrine with a dose increased to the maximum dose, together with crystalloids and albumin. In a case report of a patient with hypopituitarism who had epigastric hernioplasty, the authors described delayed awakening and persistent neuromuscular blockade in the patient, despite preoperative optimization, who needed postoperative mechanical ventilation for a day. During the procedure, they used both depth of anesthesia and neuromuscular monitoring, but the patient needed postoperative mechanical ventilation because of hypotension that required inotropes and delayed awakening from general anesthesia [7]. Therefore, it is necessary to prepare for the possibility of postoperative mechanical ventilation whenever these patients are scheduled for surgery.
Conclusions
We report a case of SS in a 56-year-old woman undergoing a major surgery. Healthcare providers should be aware of the perioperative risk of SS. No consensus, guidelines, or randomized trials for the safe perioperative management of patients with SS have been identified by a thorough review of the literature.
Learning points
The perioperative care of patients with SS necessitates the utmost caution in addition to successful management based on close coordination between the endocrinologist, surgeon, and anesthetist.
Declaration of patient consent: The author certifies that. They were assured that the patients' names and initials will not be published and though every effort will be made to conceal the patient's identity, anonymity cannot be guaranteed.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The author declares no conflict of interest.
Informed Consent
All appropriate consent forms were obtained from the patient for the publication of the case report. Consent was also given for images and other clinical information to be reported in the journal.
Author Contributions
Rania Naguib: concept, design, literature search, data acquisition, manuscript preparation, manuscript editing and manuscript review.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
SS: Sheehan’s syndrome; TSH: thyroid-stimulating hormone; Free T4: free thyroxine; ACTH: adrenocorticotropic hormone
| References | ▴Top |
- Olmes GL, Solomayer EF, Radosa JC, Sklavounos P, Agne P, Schunk SJ, Haj Hamoud B. Acute Sheehan's syndrome manifesting initially with diabetes insipidus postpartum: a case report and systematic literature review. Arch Gynecol Obstet. 2022;306(3):699-706.
doi pubmed - Zain A, Sivakumar A, Akah O, Shiza ST, Mahadevaiah A, Khan A. A rare case of Sheehan syndrome with cardiac tamponade. Cureus. 2022;14(4):e24329.
doi - Thompson CJ, Costello RW, Crowley RK. Management of hypothalamic disease in patients with craniopharyngioma. Clin Endocrinol (Oxf). 2019;90(4):506-516.
doi pubmed - Genetu A, Anemen Y, Abay S, Bante SA, Mihrete KM. A 45-year-old female patient with Sheehan's syndrome presenting with imminent adrenal crisis: a case report. J Med Case Rep. 2021;15(1):229.
doi pubmed - Sadiq S, Chowdhury A. A case of Sheehan syndrome 7 years postpartum with transaminitis and hyperlipidemia. Am J Case Rep. 2021;22:e930908.
doi pubmed - Matsuzaki S, Endo M, Ueda Y, Mimura K, Kakigano A, Egawa-Takata T, Kumasawa K, et al. A case of acute Sheehan's syndrome and literature review: a rare but life-threatening complication of postpartum hemorrhage. BMC Pregnancy Childbirth. 2017;17(1):188.
doi pubmed - Choudhuri R, Sandeep K, Adhikari D, Sinha S. Anaesthetic management of a dwarf with hypopituitarism presenting for epigastric hernioplasty: A case report. J Metabolic Synd. 2014;3(154):2167-0943.1000154.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
