| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Review
Volume 12, Number 6, December 2022, pages 161-167
Protective Effect of Metformin on Venous Thrombosis in Diabetic Patients: Findings From a Systematic Review
Sultan Alqahtania, b, e , Moeber Mahzarib, c, d
aDepartment of Basic Medical Sciences, College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
bKing Abdullah International Medical Research Center (KAIMRC), Riyadh, Saudi Arabia
cCollege of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
dDepartment of Medicine, Ministry of National Guard Health Affairs, Riyadh, Saudi Arabia
eCorresponding Author: Sultan Alqahtani, Department of Basic Medical Sciences, College of Medicine, King Saud bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Manuscript submitted October 25, 2022, accepted December 13, 2022, published online December 30, 2022
Short title: Effect of Metformin on VTE in DM Patients
doi: https://doi.org/10.14740/jem848
- Abstract
- Introduction
- Materials and Methods
- Study Results
- Discussion
- Conclusion and Implications for Future
- References
| Abstract | ▴Top |
Background: Despite the effects of metformin on cardiovascular diseases, there is limited evidence supporting its beneficial effects on venous thrombosis, and such evidence is not qualitatively synthesized both from observational and intervention studies, thereby limiting our understanding of the role of metformin in preventing venous thromboembolism (VTE). Thus, we carried out a systematic review of the epidemiological studies assessing the role of metformin in preventing VTE among diabetic patients.
Methods: A systematic search of three main electronic databases including Embase, PubMed, and EBSCO was undertaken in 2021. Any study conducted between 2000 and 2021 that addressed the role of metformin in preventing venous thrombosis in patients diagnosed with type 2 diabetes mellitus was considered eligible.
Results: Following a comprehensive review of the research articles based on the eligibility criteria, six articles were incorporated into the review. The findings of the review demonstrate that metformin was found to be associated with 22% to 58% risk reduction for venous thrombosis among diabetic patients. However, due to the observational studies included in the meta-analysis, the protective effect may not be independent of other risk factors or other variables.
Conclusion: Overall, the findings showed a beneficial effect of metformin against venous thrombosis, meaning that metformin may play a vital role in preventing deep venous thrombosis among patients diagnosed diabetes mellitus. However, future studies are warranted before making any conclusions about the efficacy of metformin against venous thrombosis in diabetic patients.
Keywords: Metformin; Venous thrombosis; Diabetes mellitus
| Introduction | ▴Top |
Vascular disease including venous thromboembolism (VTE) is a common cause of death among patients with comorbid conditions such as diabetes mellitus [1, 2]. VTE results in a range of events from symptomless distal venous thrombus of deep veins to threatening deep venous thrombus and fatal pulmonary embolism [3]. The likelihood of VTE and its associated complications are higher in older patients than younger ones and the risk becomes two-fold with every decade of aging [4]. This risk also varies by the sex of the patients with males being affected more by the second episode than females. The yearly incidence of VTE is between 1.5 and 3.0 cases per 1,000 individuals. The incidence of VTE is even higher among diabetic patients. For example, the data suggest the annual rate of VTE among diabetic patients was 432 per 100,000 population [2]. VTE is considered as the third most common cause of cardiovascular disease following stroke and myocardial infarction [3, 5].
It seems that metformin being an antihyperglycemic drug prevents cardiovascular disease beyond glycemic control [6]. However, despite the effects of metformin on glycemic control, its effects on venous thrombosis may be different. Overall, there is limited evidence supporting such beneficial effects with scarce evidence from well-conducted trials. Few epidemiological studies have shown that hypoglycemic agents such as metformin may have a direct effect on VTE [7]. However, such evidence is not qualitatively synthesized both from observational and intervention studies, thereby limiting our understanding of the role of metformin in preventing VTE. Thus, we carried out a systematic review of the epidemiological studies assessing the role of metformin in preventing VTE. The findings of this review will help clinicians and researchers to plan further studies and make evidence-based clinical and policy decisions to treat the patients appropriately and reduce the burden of VTE and its associated morbidity and mortality.
| Materials and Methods | ▴Top |
Searching strategy
The updated Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) was employed to carry out this systematic review on assessing the role of metformin in preventing VTE [8]. A systematic search of three main electronic databases including Embase, PubMed, and EBSCO was undertaken. Additionally, using two techniques such as snowballing and pearl growing methods, relevant articles were also searched and reviewed [9, 10]. All relevant published articles from January 2001 to December 2021 were included and we limited the search to articles published in the English language due to translation issues in other languages. Search restrictions with filters were employed on the language (English), publication period, and age category to include eligible studies in the search.
Using different combinations of keywords and after conducting a deep literature search by using the following search terms: “Metformin AND venous thrombus AND Diabetes”, “Metformin AND thrombus formation AND Diabetes”, “Metformin AND thromboembolism AND Diabetes Mellitus”, metformin AND deep vein thrombosis AND prediabetes”, and “Metformin AND thromboembolism OR thrombus AND Diabetes Mellitus”. In addition, the most prevalent concepts were employed including metformin AND venous thrombus. Then these major concepts were combined using combinations (AND, OR) relevant to the research question. An example of a complete search strategy included: “Metformin AND thromboembolism OR thrombus AND Diabetes Mellitus OR Type 2 Diabetes Mellitus” ((“metformin”/exp OR metformin) AND (“thromboembolism”/exp OR thromboembolism) OR “thrombus”/exp OR thrombus) AND (“diabetes mellitus”/exp OR “diabetes mellitus” OR ((“diabetes”/exp OR diabetes) AND mellitus)). Further, truncation (*) with a similar root word was employed to identify more germane articles.
Study selection
Any study that focused on the role of metformin in preventing VTE in patients diagnosed with type 2 diabetes mellitus was considered eligible to be included in the review. We considered both observational and interventional studies that had assessed the beneficial role of metformin in preventing VTE formation among diabetic patients. However, grey literature, review articles, qualitative studies, letters to the editor, secondary data, and case reports were excluded from this review. The main outcome of interest was VTE in diabetic patients and to include the maximum literature on this topic, we considered both descriptive and analytical observational studies.
Data extraction
Data extraction was carried out independently. Initially, all appropriate research studies were imported into the reference manager software, where an individual study was reviewed, and all duplicate studies were discarded. As a first step, the chosen articles were screened by titles, then by abstracts, and finally, a full-text articles evaluation was carried out. The following information was extracted in the chosen observational studies: research author, reference of the study, year of publication, country, total sample size, gender of the study participants, age group, key findings, and main conclusion of the studies. The abstracts that did not explicitly explore the study objective were not reviewed further and this was followed by retrieving and reviewing the full-text articles of the appropriate. A standardized proforma was used to abstract and summarize the articles that met the required eligibility criteria. In addition, the references of all relevant studies were also assessed to evade missing any useful studies.
| Study Results | ▴Top |
A total of 8,879 records were identified in three databases (Embase, PubMed, and EBSCO). After removing 4,578 duplicates, the remaining 4,301 unique studies were left whose titles and abstracts were screened. During this process of reviewing abstracts, 186 articles did not meet the eligibility criteria based on the abstract reading, and 34 articles were not considered potentially eligible after reviewing full documents. Following a comprehensive review of the research articles based on the eligibility criteria, six articles were incorporated in the review as shown in Figure 1.
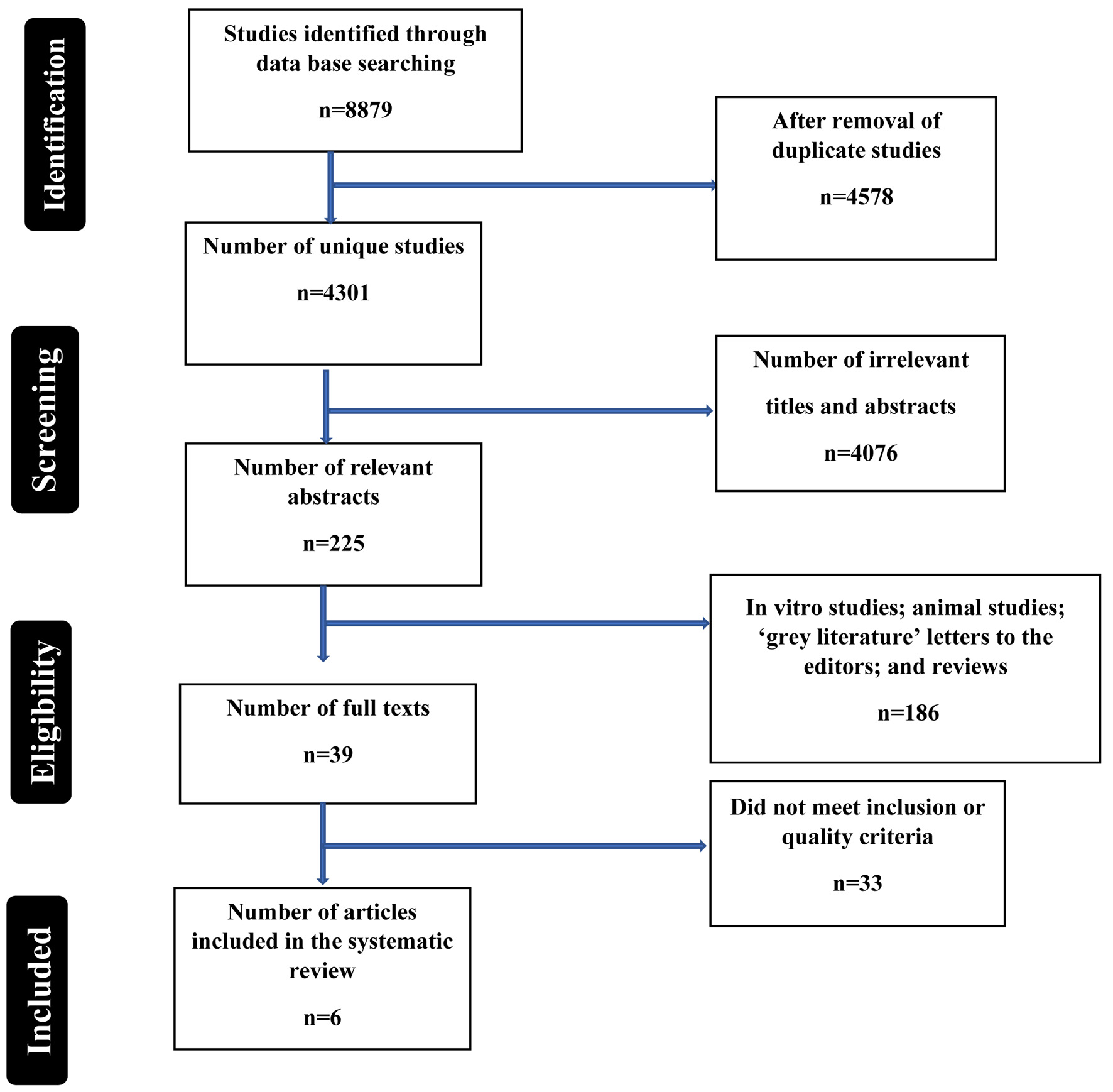 Click for large image | Figure 1. Flow chart summarizing the identification and selection of relevant papers. |
Study characteristics
Studies were conducted in different countries across the world such as Taiwan, Saudi Arabia, Sudan, and Turkey (Table 1 [11-16]). Overall, the sample size of the included studies was reasonable ranging from 24 to 907,277 diabetic patients. Regarding the gender distribution of the -participants, the findings revealed that both males and females equally participated in the respective studies. Almost all of the studies were observational studies except one randomized controlled trial and majority of the studies mentioned their outcome, which was mainly VTE or thrombus formation or mortality in diabetic patients.
 Click to view | Table 1. Characteristics of the Included Studies in the Systematic Review (n = 6) |
Summary of the key findings included in the review
Overall, the results revealed a favorable effect of metformin against deep venous thrombosis, meaning that metformin may play a vital role in preventing deep venous thrombosis among patients (Table 2). For example, a non-randomized, pair-matched cohort study was undertaken in Taiwan in 2014 on 14,945 diabetic patients [14]. Of these 7,167 patients were taking metformin and the remaining 7,778 were in the control group. The cohort of diabetic patients was followed for 3.74 years and it was found that out of 7,167 patients given metformin, 0.21% developed deep venous thrombosis while 0.56% from the control group [14]. Patients who received metformin were 58% less likely to develop venous thrombosis than those who did not receive metformin with significant results (hazard ratio (HR): 0.42, 95% confidence interval (CI): 0.240 - 0.758) [14]. One more prospective cohort study was conducted in Saudi Arabia on 277 patients diagnosed with venous thrombosis [12]. After the average time of follow-up of 1 year, it was found that metformin reduced the risk of thrombosis by 84% (HR: 0.78, 95% CI: 0.65 - 0.95) among elderly patients after adjusting for other variables in the model [12]. Likewise, a cross-sectional study was conducted in Khartum-Sudan on 96 diabetic patients. These patients were either given metformin or glimperide and effects were seen on platelet indices such as mean platelet volume, platelet large cell ratio, and platelet distribution width [11]. The findings revealed that both types of treatments were found to reduce the platelet indices with insignificant results for glimperide [11]. Both metformin and glimperide were shown to have a favorable prognostic effect on pro-thrombotic state. However, metformin was found to have a much better effect on platelet indices than glimperide [11].
 Click to view | Table 2. Summary of Findings From the Included Studies in the Systematic Review (n = 6) |
A large nationwide prospective cohort study was conducted in Taiwan using the data of 907,277 patients with the age up to 104 years [13]. The subjects were followed for about 10.4 years and various risk and protective factors were identified for the retinal vein occlusion. The study findings demonstrated that metformin was found to be protective against retinal vein occlusion among diabetic patients [13]. More precisely, it reduced the risk of retinal vein occlusion by 54% after adjusting for demographic and clinical factors (HR: 0.46, 95% CI: 0.30 - 0.71) [13]. These findings are consistent with a national primary care database study conducted in London in 2019 [17]. Likewise, a prospective open-labeled study was conducted in diabetic patients; however, the sample size was only 24. The study findings showed that metformin reduced the formation of plasminogen activator inhibitors and vascular endothelial growth factors [16]. After 4 weeks of follow-up, metformin was found to improve endothelial function and prevent thrombus formation. However, there was no effect on chronic subclinical vascular formation among obese insulin-resistant diabetic individuals [16]. Likewise, a study was conducted to examine the effects of metformin in 38 patients diagnosed with type 2 diabetes mellitus in a double-blinded randomized controlled trial. Patients were followed for about 6 weeks after being randomized to metformin and placebo [15]. Among those who were treated with metformin, basal and post-venous occlusion plasminogen activator inhibitor fell after 3 weeks without any change in these concentrations in the placebo group. After 3 weeks, post venous occlusion for plasminogen activator activity increased in the metformin group [15].
| Discussion | ▴Top |
This review was undertaken to summarize the evidence regarding the protective effect of metformin on VTE in diabetic patients. Overall the findings of the review demonstrated a protective effect of metformin among diabetic patients in terms of reducing venous thrombus formation. Though, limited evidence exists and perhaps there is a need to conduct more randomized controlled trials, the available evidence is suggestive of beneficial effects of metformin against VTE. This can be further confirmed by undertaking large intervention studies to endorse the findings.
According to the current guidelines of the American Diabetes Association/European Association, metformin should be considered as either as a monotherapy or in combination for patients diagnosed with type 2 diabetes mellitus. This is even more beneficial for patients who are at risk of thrombus formation. Metformin being an insulin sensitizer can improve the function of vessels and related vascular abnormalities with few side effects in patients with type 2 diabetes mellitus [18]. The potential mechanisms by which metformin may prevent venous thrombosis are by inhibiting platelet activation in vivo and in vitro [19]. The evidence suggests that platelets are involved in several biological processes such as clotting, vascular lesions, and activation of other platelets [20]. This activity of platelets is markedly suppressed in the presence of metformin and it is mainly by suppression of platelet prothrombinase activity and by reducing extracellular mitochondrial release [1, 19].
This is consistent with the reduced platelet adhesive function after administering metformin. The animal studies suggest that metformin significantly suppressed aggregation of platelets and prevent both arterial and venous thrombosis in rat models [19]. And thrombus formation deteriorated in the rats treated with metformin [19]. Besides, it has been found that metformin reduces the size and weight of arterial and venous thrombi and subsequently reduces the incidence of pulmonary embolism [19]. Also, metformin reduces markers of endothelial activation such as Von Willebrand factor and it also decreases the inflammation and levels of plasminogen activator inhibitor 1 [19, 21-23]. These potential mechanisms contribute to the protective effect of metformin in reducing thrombus formation and associated mortality in diabetic patients.
Strengths and limitations
This is a unique review as it is the first of its type that synthesized the findings of the role of metformin in preventing thromboembolism or associated mortality in diabetic individuals. The findings of this review can provide a framework to clinicians, endocrinologists, and policymakers to use metformin among diabetic patients who are at risk of developing thrombus formation to reduce morbidity and mortality mainly in the elderly. We also used an updated PRISMA checklist to conduct this review and most of the studies were large enough to be adequately powered to detect the protective effect of metformin on VTE. Besides, we included studies mainly from high-middle income countries, therefore, findings may not be generalizable to resource poor-settings with differences in the prevalence of causal partners or other factors that may interact with metformin differently in different settings.
Despite these strengths, the findings of the current review should be interpreted with caution due to some caveats associated with the individual studies. Since most all of the studies were observational epidemiological studies, one cannot establish causality between metformin and the outcome under investigation. Since the observational studies suffer from issues of unmeasured confounding, therefore, the researchers could not collect data on all confounders or covariates in their individual studies. Hence, the effect of metformin cannot be independent of all the factors. To address this issue, it is recommended to undertake randomized controlled trials in the future to prove the preventive effect of metformin independent of other factors. In addition, due to the overall dearth of literature on this area, studies from low-middle income countries were almost negligible, which warrant conducting more such studies in resource-poor settings. Also, the overall sample size of the review was small due to the scarcity of research in this area. Despite performing a deep literature search, we could not find more articles relevant to the study objective, which implies undertaking more research in this area before making any firm conclusions. Lastly, the included studies were of varying sample sizes, which is unavoidable but almost all of the studies were able to detect the desired effect size of metformin against VTE. However, overall, the included studies were very few as the literature is scarce on this topic mainly in human beings and most of the evidence is from animal or laboratory studies. These warrants conducting more epidemiological studies in human beings before making any robust conclusions about the role of metformin against thrombus formation in diabetic patients.
| Conclusion and Implications for Future | ▴Top |
Overall, the existing studies included in this review demonstrate that metformin may be found protective against VTE, mainly in diabetic patients. Based on the available findings, metformin may be safely used in diabetic patients at risk of thromboembolism; however, we would recommend conducting more epidemiological studies particularly randomized controlled trials to assess the effect of metformin on VTE before making any definitive conclusions about the same. Considering the limited sample size of this review, more studies and their respective reviews are required to confirm these findings and these studies need to be undertaken both in developing and developed countries to confirm these findings and recommend the use of metformin on a broader scale for the prevention of thromboembolism in diabetic patients.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Not applicable.
Author Contributions
Both authors contributed equally to conceptualization; data curation; formal analysis; funding acquisition; investigation; methodology; project administration; resources; software; supervision; validation; visualization; roles/writing process. Both authors involve in the writing of the original draft; review and editing processes.
Data Availability
The data used to support the findings of this study are included within the article.
| References | ▴Top |
- Influence of diabetes on 5-year mortality and morbidity in a randomized trial comparing CABG and PTCA in patients with multivessel disease: the Bypass Angioplasty Revascularization Investigation (BARI). Circulation. 1997;96(6):1761-1769.
doi pubmed - Petrauskiene V, Falk M, Waernbaum I, Norberg M, Eriksson JW. The risk of venous thromboembolism is markedly elevated in patients with diabetes. Diabetologia. 2005;48(5):1017-1021.
doi pubmed - Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, Cook DJ, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e195S-e226S.
doi pubmed - Stein PD, Hull RD, Kayali F, Ghali WA, Alshab AK, Olson RE. Venous thromboembolism according to age: the impact of an aging population. Arch Intern Med. 2004;164(20):2260-2265.
doi pubmed - Anderson FA, Jr., Wheeler HB, Goldberg RJ, Hosmer DW, Patwardhan NA, Jovanovic B, Forcier A, et al. A population-based perspective of the hospital incidence and case-fatality rates of deep vein thrombosis and pulmonary embolism. The Worcester DVT Study. Arch Intern Med. 1991;151(5):933-938.
doi pubmed - Driver C, Bamitale KDS, Kazi A, Olla M, Nyane NA, Owira PMO. Cardioprotective effects of metformin. J Cardiovasc Pharmacol. 2018;72(2):121-127.
doi pubmed - Han Y, Xie H, Liu Y, Gao P, Yang X, Shen Z. Effect of metformin on all-cause and cardiovascular mortality in patients with coronary artery diseases: a systematic review and an updated meta-analysis. Cardiovasc Diabetol. 2019;18(1):96.
doi pubmed - Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
doi pubmed - Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005;331(7524):1064-1065.
doi pubmed - Schlosser RW, Wendt O, Bhavnani S, Nail-Chiwetalu B. Use of information-seeking strategies for developing systematic reviews and engaging in evidence-based practice: the application of traditional and comprehensive Pearl Growing. A review. Int J Lang Commun Disord. 2006;41(5):567-582.
doi pubmed - Hussein HA, Babikir DM, Elmagzoub FMA, Samaan MA. The effect of metformin and glimepiride on platelet count and indices among diabetic patients attending Jaber Abu Aliz Diabetic Center in Khartoum State. Research Square;2021.
doi - Aleidan FAS. The Cumulative Incidence and Risk Factors of Recurrent Venous Thromboembolism in the Elderly. Vasc Health Risk Manag. 2020;16:437-443.
doi pubmed - Lin TC, Hwang DK, Hsu CC, Peng CH, Wang ML, Chiou SH, Chen SJ. Protective effect of metformin against retinal vein occlusions in diabetes mellitus - A nationwide population-based study. PLoS One. 2017;12(11):e0188136.
doi pubmed - Lu DY, Huang CC, Huang PH, Chung CM, Lin SJ, Chen JW, Chan WL, et al. Metformin use in patients with type 2 diabetes mellitus is associated with reduced risk of deep vein thrombosis: a non-randomized, pair-matched cohort study. BMC Cardiovasc Disord. 2014;14:187.
doi pubmed - Grant PJ, Stickland MH, Booth NA, Prentice CR. Metformin causes a reduction in basal and post-venous occlusion plasminogen activator inhibitor-1 in type 2 diabetic patients. Diabet Med. 1991;8(4):361-365.
doi pubmed - Ersoy C, Kiyici S, Budak F, Oral B, Guclu M, Duran C, Selimoglu H, et al. The effect of metformin treatment on VEGF and PAI-1 levels in obese type 2 diabetic patients. Diabetes Res Clin Pract. 2008;81(1):56-60.
doi pubmed - Hinton W, et al. Metformin is associated with reduced risk of venous thromboembolism in Type 2 diabetes: a national primary care database study. Diabetic Medicine. 2019;36(S1):19.
- Madiraju AK, Erion DM, Rahimi Y, Zhang XM, Braddock DT, Albright RA, Prigaro BJ, et al. Metformin suppresses gluconeogenesis by inhibiting mitochondrial glycerophosphate dehydrogenase. Nature. 2014;510(7506):542-546.
doi pubmed - Xin G, Wei Z, Ji C, Zheng H, Gu J, Ma L, Huang W, et al. Metformin Uniquely Prevents Thrombosis by Inhibiting Platelet Activation and mtDNA Release. Sci Rep. 2016;6:36222.
doi pubmed - Barile CJ, Herrmann PC, Tyvoll DA, Collman JP, Decreau RA, Bull BS. Inhibiting platelet-stimulated blood coagulation by inhibition of mitochondrial respiration. Proc Natl Acad Sci U S A. 2012;109(7):2539-2543.
doi pubmed - de Jager J, Kooy A, Schalkwijk C, van der Kolk J, Lehert P, Bets D, Wulffele MG, et al. Long-term effects of metformin on endothelial function in type 2 diabetes: a randomized controlled trial. J Intern Med. 2014;275(1):59-70.
doi pubmed - Derosa G, Gaddi AV, Piccinni MN, Ciccarelli L, Salvadeo S, Peros E, Ghelfi M, et al. Antithrombotic effects of rosiglitazone-metformin versus glimepiride-metformin combination therapy in patients with type 2 diabetes mellitus and metabolic syndrome. Pharmacotherapy. 2005;25(5):637-645.
doi pubmed - Sobel BE, Hardison RM, Genuth S, Brooks MM, McBane RD, 3rd, Schneider DJ, Pratley RE, et al. Profibrinolytic, antithrombotic, and antiinflammatory effects of an insulin-sensitizing strategy in patients in the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial. Circulation. 2011;124(6):695-703.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
