| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Case Report
Volume 11, Number 2, April 2021, pages 49-51
Is There Any Association Between Diabetes and Intussusception in Adults? A Case Report
Arshad Mahmooda, Mohamed H. Ahmedb, d, Khalid Cannac
aDepartment of Surgery, Milton Keynes Hospital NHS Trust, Milton Keynes, UK
bDepartment of Medicine and HIV Metabolic Clinic, Milton Keynes Hospital NHS Trust, Milton Keynes, UK
cDepartment of Surgery, Bedford Hospital, Bedford, UK
dCorresponding Author: Mohamed H. Ahmed, Department of Medicine and HIV Metabolic Clinic, Milton Keynes University Hospital NHS Foundation Trust, Eagelstone, Milton Keynes, Buckinghamshire, UK
Manuscript submitted February 27, 2021, accepted March 9, 2021, published online April 25, 2021
Short title: Association Between Diabetes and Intussusception
doi: https://doi.org/10.14740/jem732
| Abstract | ▴Top |
We report a case of a 30-year-old man with insulin-dependent diabetes (type 1 diabetes) since he was 12 years old, who was admitted to our hospital with history of a sudden onset of generalized abdominal pain worst in the epigastrium which radiated to the back. The pain was described as severe, sharp and intermittent and was exacerbated by movement. He had two episodes of vomiting without any bloody content and denied fever or changes in bowel habit previously. Computed tomography scan showed the presence of intussusception, which was treated surgically. In this case report, we also provide an up-to-date discussion for the association between diabetes and intussusception.
Keywords: Diabetes; Intussusception; Adult
| Introduction | ▴Top |
Intussusception is rare in adults, and it is not surprising that it makes up just 5% of all cases of intestinal obstruction [1-3]. The classical definition is telescoping of a segment of bowel into its adjacent part [4]. In children, the cause is thought to be idiopathic, while in adults, it is likely related to a lesion that affects the gut motility [1]. Importantly, most lesions involving the colon are malignant, while those involving the small bowel are benign [5-7] and small and large bowel intussusceptions make up 90% of all cases of intussusceptions. The other 10% was attributed to postoperative structural causes secondary to jejunostomy, gastrectomy or bypass surgeries [4, 5]. The diagnosis can be difficulty as patients can present with vague symptoms. In addition, the classical triad of abdominal pain, palpable sausage-shaped mass and “current-jelly” stools is not always seen in adults. Furthermore, an average duration of symptom presentation is 7.9 days [1-7]. Patients can present with features related to intestinal obstruction, in the form of vomiting, distension and pain. The use of computed tomography (CT) as a diagnostic tool is widely accepted as the most accurate and efficacious modality of diagnosis [6, 7]. Definitive management for intussusceptions in adults is laparotomy with reduction and/or resection of the pathological bowel segment [1-7]. Diabetes was suggested to have a role in the process of formation of intussusception. In this case report, we discuss intussusception in individuals with diabetes in addition to review of the literature of an association between diabetes and intussusception.
| Case Report | ▴Top |
We report a case of a 30-year-old man known to have type 1 diabetes for 18 years and gastric reflux disease. His only medication was long and short acting insulin and occasional use of proton pump inhibitor (lansoprazole). He presented to our hospital with a sudden onset of generalized abdominal pain worst in the epigastrium which radiated to the back. The pain was described as severe, sharp and intermittent and was exacerbated by movement. He had two episodes of vomiting without any bloody content and denied fever or changes in bowel habit previously. Venous blood gas showed an elevated lactate of 4.0. On admission, plasma glucose was 14.2 mmol/L, ketone was 1.4 and pH was 7.46. Previous investigation showed well-controlled diabetes (HbA1c 6.3%) with normal renal, liver and thyroid functions. No recorded evidence of diabetes complications like nephropathy, ischemic heart disease or cerebrovascular events, retinopathy, autonomic neuropathy or peripheral neuropathy was noted. Urgent CT of abdomen/pelvis showed the presence of jejunal intussusception possibly secondary to an underlying leiomyoma (Fig. 1). There was no evidence of bowel wall ischemia or perforation, and intraabdominal organs were all unremarkable. Urgent surgical intervention was advised. He was taken to surgical theater for a laparotomy with the resection of the segment of intussusception with primary anastomosis. An attempt at manual reduction was not successful. The patient made full recovery after the operation. The histology obtained intra-operatively revealed a leiomyoma (measuring 45 × 45 × 25 mm) acting as the lead point triggering the intussusception.
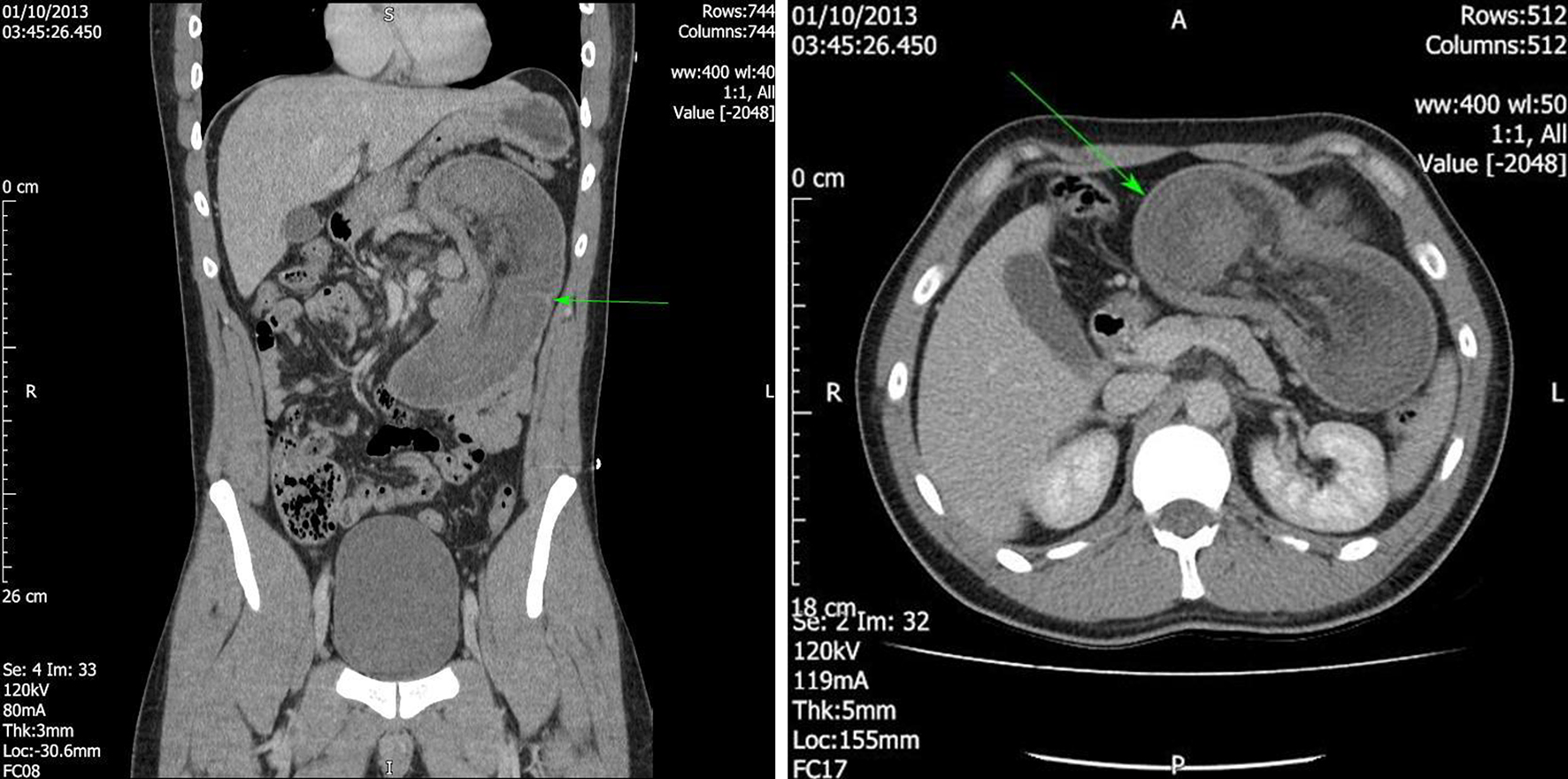 Click for large image | Figure 1. Urgent CT of abdomen/pelvis showing the presence of jejunal intussusception possibly secondary to an underlying leiomyoma (arrows). There was no evidence of bowel wall ischemia or perforation, and intraabdominal organs were all unremarkable. CT: computed tomography. |
| Discussion | ▴Top |
Diabetes can have serious impact on the gastrointestinal system, for instance, neuropathies within the enteric nervous system are associated with gastroenteropathy. In addition, the diabetes-induced enteric neuropathy can be associated with notorious symptoms like nausea, dyspepsia, vomiting, pain, dysphagic, bloating, diarrhoea, constipation and fecal incontinence [8]. The association of diabetes with intussusception was reported in several case reports. For instance, McFarlane et al showed that in a 20-year-old man with intussusception and blood glucose of 72.7 mmol/L, treatment of hyperglycemia was associated with complete resolution of intussusception in the CT scan [9]. A 23-year-old woman with type 1 diabetes also developed intussusception with onset of diabetic ketoacidosis (DKA) and the intussusception resolved with treatment of DKA [10]. Diabetes and DKA can be associated with intussusception that will require surgical interventions. For instance, Raghavan et al showed that in a case of a 23-year-old Caucasian man with DKA, three intussusceptions involving the small intestine were easily reduced manually during exploratory laparotomy [11]. Furthermore, intussusception was reported in children with diabetes [12]. Bariatric surgery in association with and without diabetes can be associated with intussusceptions [13, 14]. In this case report, the patient was known to have type 1 diabetes for 18 years. There was no record of diabetes complications or autonomic neuropathy. Factors that may predispose patients with diabetes to intussusception include altered gut motility caused by: 1) acute metabolic decompensation (i.e., hyperglycemia and/or acidosis) and/or 2) chronic hyperglycemia and/or 3) autonomic neuropathy. The long-standing duration of type 1 diabetes could be an important factor in decreasing gut motility, which can be attributed to chronic hyperglycemia [8-13]. The impact of medication on gut motility is unlikely in this patient, as he was only taking insulin and occasional use of proton pump inhibitor. The association between diabetes and intussusception and whether the presence of DKA or bariatric surgery can accelerate the process of formation of intussusception will need further research investigation.
Acknowledgments
We are grateful for our families for their continuous support.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained from the patient.
Author Contributions
All authors contributed equally in collecting data about the patient, literature review and analyzing the data, writing and approving the manuscript. Arshad Mahmood and Khalid Canna operated on the patient and established the idea of the case report.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Yakan S, Caliskan C, Makay O, Denecli AG, Korkut MA. Intussusception in adults: clinical characteristics, diagnosis and operative strategies. World J Gastroenterol. 2009;15(16):1985-1989.
doi pubmed - Bar-Ziv J, Solomon A. Computed tomography in adult intussusception. Gastrointest Radiol. 1991;16(3):264-266.
doi pubmed - Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, Kuwano H. The diagnosis and treatment of adult intussusception. J Clin Gastroenterol. 2003;36(1):18-21.
doi pubmed - Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, Hertz M. Intussusception in adults: CT diagnosis. Clin Radiol. 1998;53(1):53-57.
doi - Warshauer DM, Lee JK. Adult intussusception detected at CT or MR imaging: clinical-imaging correlation. Radiology. 1999;212(3):853-860.
doi pubmed - Azar T, Berger DL. Adult intussusception. Ann Surg. 1997;226(2):134-138.
doi pubmed - Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173(2):88-94.
doi - Meldgaard T, Keller J, Olesen AE, Olesen SS, Krogh K, Borre M, Farmer A, et al. Pathophysiology and management of diabetic gastroenteropathy. Therap Adv Gastroenterol. 2019;12:1756284819852047.
doi pubmed - McFarlane SI, Byrne K, Shin J, Williams R. Intussusception in an adult patient with severe hyperglycaemia - a case report. Diabet Med. 2002;19(7):611-614.
doi pubmed - Koh JS, Hahm JR, Jung JH, Jung TS, Rhyu SS, Moon SW, Kang MY, et al. Intussusception in a young female with Vibrio gastroenteritis and diabetic ketoacidosis. Intern Med. 2007;46(4):171-173.
doi pubmed - Raghavan P, Salon J, Rajan D. Multiple intestinal intussusceptions as a complication of severe hyperglycemia in a patient with diabetic ketoacidosis. Case Rep Endocrinol. 2012;2012:526041.
doi pubmed - Shah N, Khadilkar V, Khadilkar A, Jahagirdar R. Intussusception as a rare clinical presentation of a child with type 1 diabetes and diabetic ketoacidosis. BMJ Case Rep. 2020;13(12).
doi pubmed - Genser L, Pattou F, Caiazzo R. Retrograde jejuno-jejunal intussusception 7years after a Roux-en-Y gastric bypass. J Visc Surg. 2015;152(2):137-139.
doi pubmed - Al Sulaiti MA, Darwish A, Al Khalifa K. Intussusception after laparoscopic one anastomosis gastric bypass: A rare complication. Int J Surg Case Rep. 2019;60:270-272.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
