| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Review
Volume 9, Number 5, October 2019, pages 127-132
Differential Diagnosis of Thyrotoxicosis
Hidekatsu Yanaia, b, c
aDepartment of Diabetes, Endocrinology and Metabolism, National Center for Global Health and Medicine Kohnodai Hospital, Chiba, Japan
bDepartment of Internal Medicine, National Center for Global Health and Medicine Kohnodai Hospital, Chiba, Japan
cCorresponding Author: Hidekatsu Yanai, Department of Internal Medicine, National Center for Global Health and Medicine Kohnodai Hospital, 1-7-1 Kohnodai, Ichikawa, Chiba 272-8516, Japan
Manuscript submitted August 16, 2019, accepted August 27, 2019
Short title: Differential Diagnosis of Thyrotoxicosis
doi: https://doi.org/10.14740/jem600
- Abstract
- Introduction
- Differential Diagnosis of Hyperthyroidism
- Differential Diagnosis of Thyrotoxicosis
- Conclusion
- References
| Abstract | ▴Top |
Hyperthyroidism is characterized by increased thyroid hormone synthesis and secretion from the thyroid gland, whereas thyrotoxicosis refers to the clinical syndrome of excess circulating thyroid hormones, irrespective of the source. Thyrotoxicosis is characterized by low serum thyroid-stimulating hormone (TSH) level and elevated serum levels of free thyroxine or free triiodothyronine, or both. Therefore, thyrotoxicosis is divided into two subtypes: thyrotoxicosis with hyperthyroidism such as Graves’ disease and Plummer’s disease, and thyrotoxicosis without hyperthyroidism such as painless and subacute thyroiditis. Here, I describe the differential diagnosis of hyperthyroidism; differentiation between Graves’ disease and Plummer’s disease; differentiation between Graves’ disease with and without thyroid storm. Further, I show the differentiation among Graves’ disease, painless thyroiditis and subacute thyroiditis. I believe that the proper diagnosis leads to appropriate treatment and management of thyrotoxicosis.
Keywords: Graves’ disease; Hyperthyroidism; Scintigraphy; Subacute thyroiditis; Thyrotoxicosis
| Introduction | ▴Top |
Hyperthyroidism is characterized by increased thyroid hormone synthesis and secretion from the thyroid gland, whereas thyrotoxicosis refers to the clinical syndrome of excess circulating thyroid hormones, irrespective of the source [1] (Fig. 1). Thyrotoxicosis is characterized by low serum thyroid-stimulating hormone (TSH) level and elevated serum levels of free thyroxine (fT4) or free triiodothyronine (fT3), or both [1]. Therefore, thyrotoxicosis is divided into two subtypes: thyrotoxicosis with hyperthyroidism and thyrotoxicosis without hyperthyroidism. Thyrotoxicosis with hyperthyroidism is caused by Graves’ disease and toxic nodular goiter (Plummer’s disease), and is characterized by a high thyroid radioactive iodine uptake. Thyrotoxicosis without hyperthyroidism is caused by painless and subacute thyroiditis, iodine-induced and drug-induced thyroid dysfunction, and factitious ingestion of excess thyroid hormones. Thyrotoxicosis due to thyroiditis is induced by a release of preformed thyroid hormones into the circulation, and this type of thyrotoxicosis is characterized by a low thyroid radioactive iodine uptake.
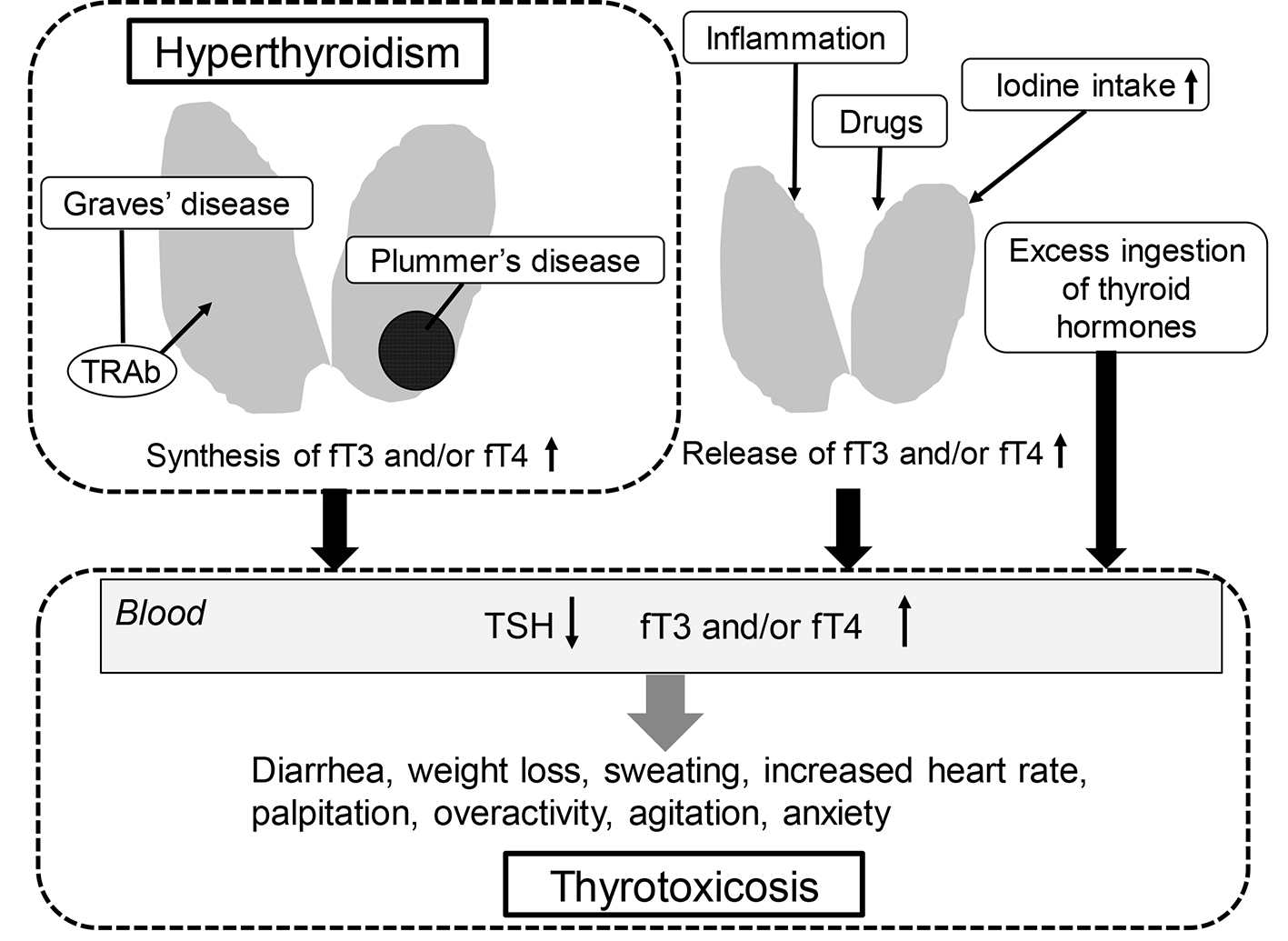 Click for large image | Figure 1. Thyrotoxicosis with and without hyperthyroidism. fT3: free triiodothyronine; fT4: free thyroxine; TRAb: anti-TSH receptor antibody; TSH: thyroid-stimulating hormone. |
The most common cause of hyperthyroidism in iodine-sufficient areas is Graves’ disease [1]. Although in iodine-sufficient areas about 80% of patients with hyperthyroidism have Graves’ disease, Plummer’s disease accounts for 50% of all cases of hyperthyroidism in iodine-deficient areas [2]. Plummer’s disease is also called toxic multinodular goiter, hyperfunctioning thyroid nodule and autonomously functioning thyroid nodule. In iodine deficient areas, chronic stimulation by TSH causes multinodular autonomous growth and function.
In Japan, Graves’ disease, painless thyroiditis and subacute thyroiditis are important in the differential diagnosis for thyrotoxicosis. An appropriate treatment for thyrotoxicosis requires an accurate diagnosis. Here, I describe how to differentiate each disease which induces thyrotoxicosis by introducing our studies.
| Differential Diagnosis of Hyperthyroidism | ▴Top |
Differentiation between Graves’s disease and Plummer’s disease
Plummer’s disease presents marked enlargement of the thyroid gland (goiter), firm thyroid nodules, and overproduction of thyroid hormone (hyperthyroidism). Incidence of Plummer’s disease among Japanese is very low, accounting for 0.5-0.8% of all thyroid nodules and 0.3% of all thyrotoxic patients [3]. The prevalence of toxic multinodular goiter (Plummer’s disease) has been reported to account for about < 1.0% of hyperthyroidism [4].
Therefore, in Japan, it is important to make a definitive diagnosis of Graves’ disease in the differential diagnosis of hyperthyroidism. We retrospectively picked up patients who had been diagnosed as having Graves’ disease, at National Center for Global Health and Medicine Kohnodai Hospital, between January 2010 and October 2018 [5]. According to the guideline for the diagnosis of Graves’ disease presented by the Japan Thyroid Association, we diagnosed patients as having Graves’ disease by observing signs of thyrotoxicosis, elevation in serum fT4 and fT3 levels, suppression of TSH and positive for anti-TSH receptor antibody (TRAb). Such a patient shall be said probably to have Graves’ disease by this guideline. We found 74 Graves’ disease patients [5], and observed 73 Graves’ disease patients except for one patient who showed positive for TRAb, suggesting an importance of measurement of TRAb for diagnosis of Graves’ disease. We previously experienced a Graves’ disease patient showing the absence of TRAb, whose Graves’ disease was diagnosed by using scintigraphy [6]. As shown in Figure 2, thyroid scintigraphy demonstrated diffuse and remarkably elevated uptake of 123I, suggesting a diagnosis of Graves’ disease.
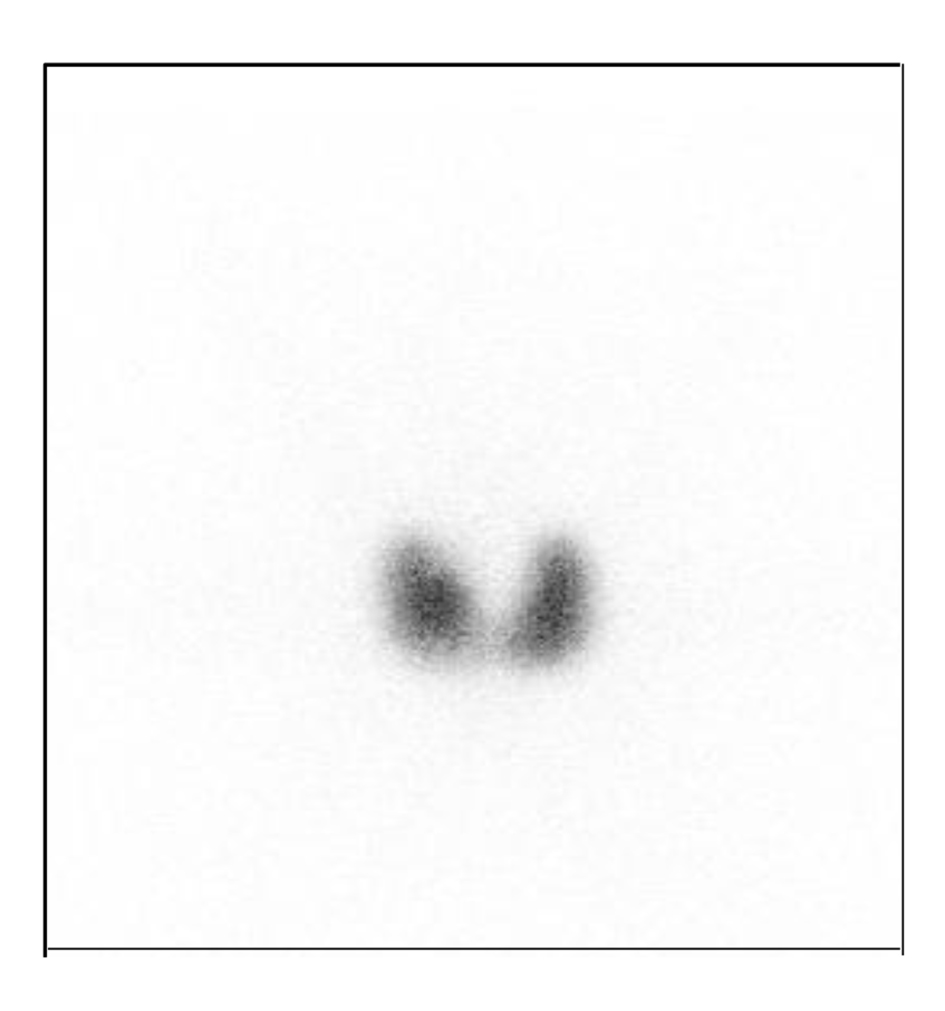 Click for large image | Figure 2. Scintigraphic finding in a patient with Graves’ disease. Diffuse uptake of 123I uptake by thyroid glands is observed in patients with Graves’ disease. |
Typical scintigraphic patterns of thyroid diseases showing thyrotoxicosis were shown in Figure 3. As shown in Figure 3a, in patients with Graves’ disease, thyroid scintigraphy demonstrates diffuse and remarkably elevated uptake of 123I. If the patient with thyrotoxicosis who showed negative for TRAb and showed scintigraphic pattern b or c, we should consider the patient having Plummer’s disease. Thyroiditis is characterized by a low thyroid radioactive iodine uptake (Fig. 3d).
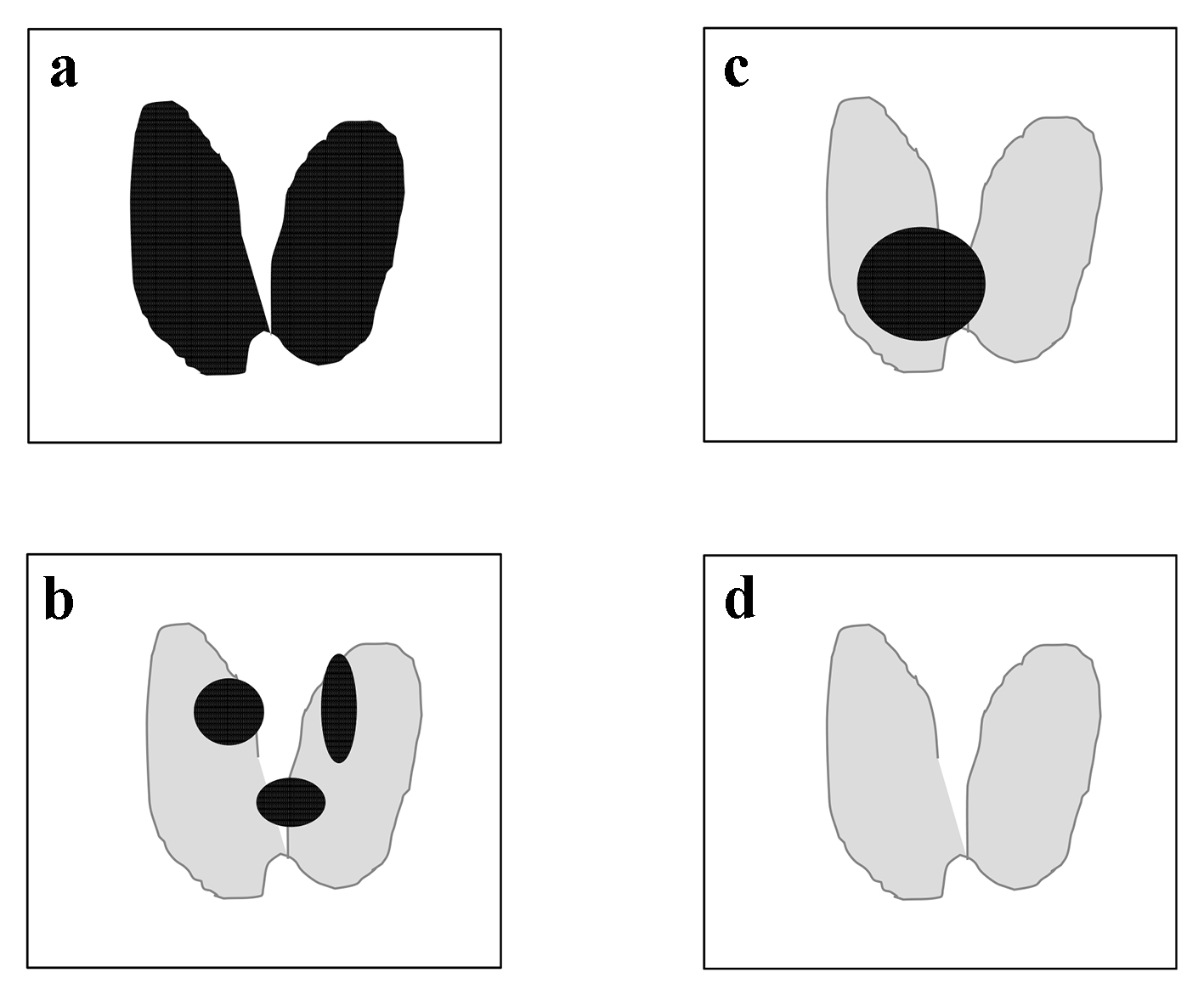 Click for large image | Figure 3. Typical scintigraphic pattern in patients with Graves’ disease (a), Plummer’s disease (b, c) and painless and subacute thyroiditis (d). Black area indicate uptake of 123I uptake. |
When we consider hyperthyroidism based on thyroid ultrasound, increased thyroid blood flow in whole thyroids (Fig. 4) in patients with hyperthyroidism suggests the existence of Graves’ disease. When we find nodules showing increased thyroid blood flow in TRAb-negative patients with hyperthyroidism, we consider such patients likely having Plummer’s disease.
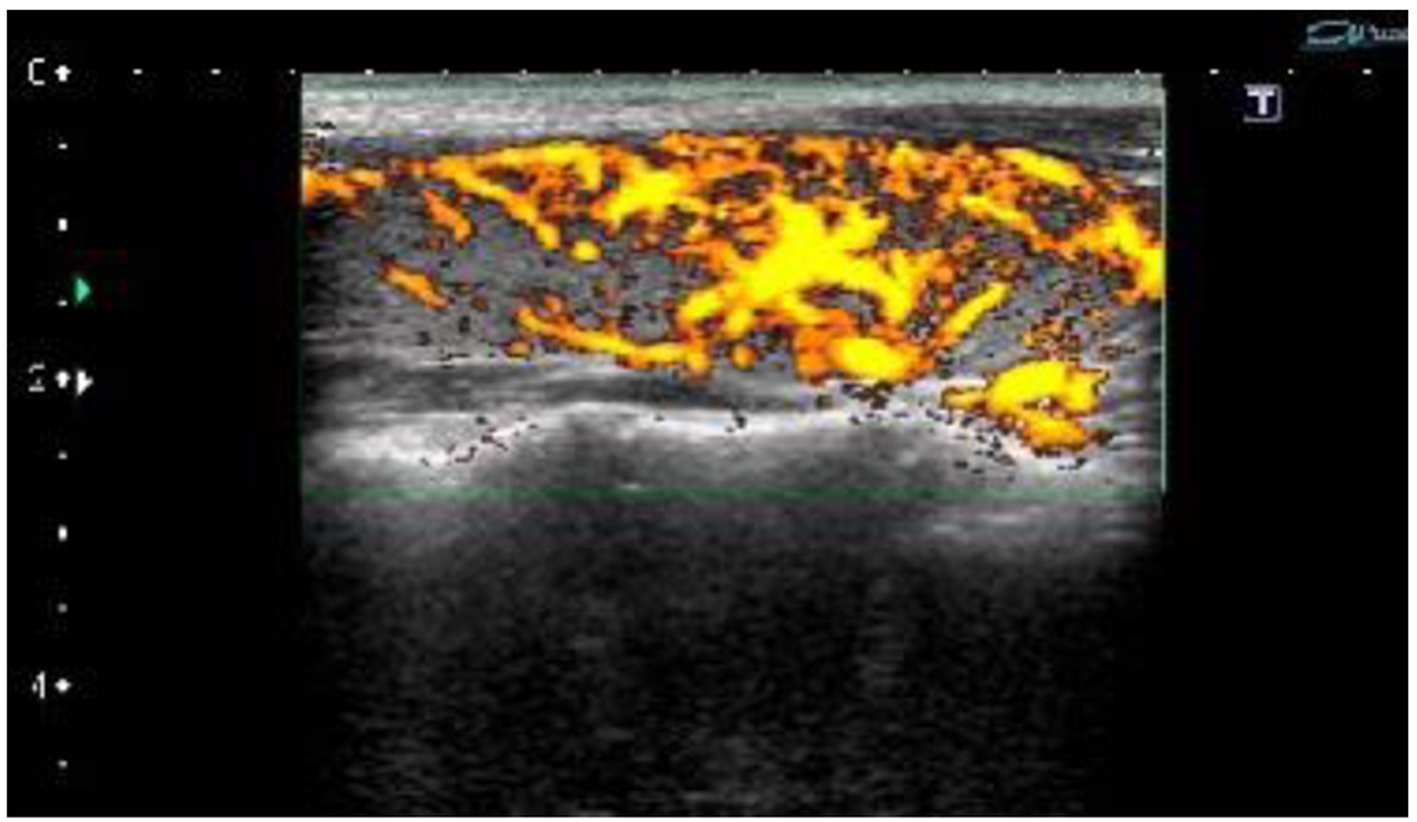 Click for large image | Figure 4. Ultrasound finding in a patient with Graves’ disease. Increased thyroid blood flow in whole thyroids is observed in a patient with Graves’ disease. |
Differentiation between Graves’s disease with and without thyroid storm (TS)
TS is very rare, however, a life-threatening medical condition requiring emergency treatment [7-9]. The incidence rate of TS was estimated to be 0.20 persons per 100,000 population per year in Japan, accounting for 0.22% of all thyrotoxic patients and 5.4% of hospitalized thyrotoxic patients [9, 10]. The mortality rate of patients with TS was 10.7% [9]. The most common causes of death in patients with TS were multiple organ failure (MOF) and congestive heart failure (CHF) [9, 11], which were induced by the decompensation of multiple organs due to thyrotoxicosis.
Since TS is rare, the criteria by Japan Thyroid Association were mainly based on information obtained from the literatures [12]. TS was defined as thyrotoxicosis plus at least one central nervous system (CNS) manifestation and one of the followings: fever (≥ 38 °C), tachycardia (≥ 130/min), CHF, or gastrointestinal (GI)/hepatic manifestation; thyrotoxicosis and at least three of the followings: fever, tachycardia, CHF, or GI/hepatic manifestations [13], however, which did not show any laboratory data including the values of TSH, fT3 and fT4.
To obtain a more objective diagnostic tool for TS, we retrospectively studied clinical, biochemical, hematological, endocrinological and immunological differences between Graves’ disease patients with and without TS at the National Center for Global Health and Medicine Kohnodai Hospital, Japan [5]. We found that patients with TS showed higher levels of both fT3 and fT4 as compared with Graves’ patients without TS (Table 1 [5]). Furthermore, we found neutrophilic leukocytosis together with eosinopenia, monocytopenia and lymphocytopenia as the characteristics for TS. We also discovered significantly higher serum alkaline phosphatase levels, and lower serum levels of triglyceride, high-density lipoprotein-cholesterol, and low-density lipoprotein-cholesterol in patients with TS as compared with those without TS. A significantly higher titer of TRAb was also characteristic for TS.
 Click to view | Table 1. Characteristics for Thyroid Storm |
| Differential Diagnosis of Thyrotoxicosis | ▴Top |
Differentiation among Graves’ disease (thyrotoxicosis with hyperthyroidism), painless thyroiditis and subacute thyroiditis (thyrotoxicosis without hyperthyroidism)
In Japan, Graves’ disease, painless thyroiditis and subacute thyroiditis are important in the differential diagnosis for thyrotoxicosis. We retrospectively picked up patients who had been diagnosed as having Graves’ disease, painless thyroiditis and subacute thyroiditis who showed thyrotoxicosis, at National Center for Global Health and Medicine Kohnodai Hospital, between January 2010 and October 2018 [14]. The guideline for diagnosis of painless thyroiditis by Japan Thyroid Association includes thyrotoxicosis without pain of the thyroid gland and spontaneous improvement of thyrotoxicosis, elevation of serum fT4, suppression of TSH and negative for TRAb. A patient showing such findings shall be said probably to have painless thyroiditis by the guideline. If decreased radioactive iodine uptake to the thyroid gland is observed in a patient, the patient has satisfied all criteria. The guideline for diagnosis of subacute thyroiditis includes a swelling with pain and tenderness in the thyroid gland, elevation of C-reactive protein (CRP), elevation of serum fT4 and suppression of TSH. A patient showing such findings shall be said probably to have subacute thyroiditis. If hypoechoic lesion at a painful portion of the thyroid gland is confirmed by ultrasonography in a patient, the patient has satisfied all criteria. In the guideline for Graves’ disease, the fT3/fT4 ratio is helpful to exclude painless thyroiditis.
Differences in clinical, endocrinological, immunological and biochemical findings and diagnostic imaging among Graves’ disease, subacute thyroiditis and painless thyroiditis were shown in Table 2 [14]. As newly obtained findings, levels of fT3 and fT4 and the fT3/fT4 ratio were higher in the order of Graves’ disease, subacute thyroiditis and painless thyroiditis. Further, leukocytosis was observed in patients with subacute thyroiditis. High positive rate and values of CRP was characteristic finding for subacute thyroiditis.
 Click to view | Table 2. Differences in Clinical, Endocrinological, Immunological and Biochemical Findings and Diagnostic Imaging Among Graves’ Disease, Subacute Thyroiditis and Painless Thyroiditis |
| Conclusion | ▴Top |
I described the differential diagnosis of hyperthyroidism; differentiation between Graves’s disease and Plummer’s disease; differentiation between Graves’s disease with and without thyroid storm. Further, I presented the differentiation among Graves’s disease, painless thyroiditis and subacute thyroiditis. I believe that the proper diagnosis leads to appropriate treatment and management of thyrotoxicosis.
Acknowledgments
I thank the staffs (Yukie Kawamura, Keiko Nakamura, Harue Aoki and Ayano Sakakibara) of the Division of Research Support, National Center for Global Health and Medicine Kohnodai Hospital.
Financial Disclosure
Author has no financial disclosures to report.
Conflict of Interest
The author declares that he has no conflict of interest concerning this article.
Author Contributions
HY designed the research, and collected and analyzed data. HY wrote and approved the final paper.
| References | ▴Top |
- De Leo S, Lee SY, Braverman LE. Hyperthyroidism. Lancet. 2016;388(10047):906-918.
doi - Laurberg P, Cerqueira C, Ovesen L, Rasmussen LB, Perrild H, Andersen S, Pedersen IB, et al. Iodine intake as a determinant of thyroid disorders in populations. Best Pract Res Clin Endocrinol Metab. 2010;24(1):13-27.
doi pubmed - Kasagi K. [Epidemiology of thyroid tumors: effect of environmental iodine intake]. Nihon Rinsho. 2007;65(11):1953-1958.
- Fukada S. [Toxic multinodular goiter]. Nihon Rinsho. 2006;64(12):2227-2232.
- Yanai H, Hakoshima M, Katsuyama H. Clinical, biochemical, hematological, endocrinological and immunological differences between Graves' disease patients with and without thyroid storm. J Clin Med Res. 2019;11(6):452-457.
doi pubmed - Hamasaki H, Yoshimi T, Yanai H. A patient with Graves' disease showing only psychiatric symptoms and negativity for both TSH receptor autoantibody and thyroid stimulating antibody. Thyroid Res. 2012;5(1):19.
doi pubmed - Gavin LA. Thyroid crises. Med Clin North Am. 1991;75(1):179-193.
doi - Tietgens ST, Leinung MC. Thyroid storm. Med Clin North Am. 1995;79(1):169-184.
doi - Akamizu T, Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, et al. Diagnostic criteria, clinical features, and incidence of thyroid storm based on nationwide surveys. Thyroid. 2012;22(7):661-679.
doi pubmed - Isozaki O, Satoh T, Wakino S, Suzuki A, Iburi T, Tsuboi K, Kanamoto N, et al. Treatment and management of thyroid storm: analysis of the nationwide surveys: The taskforce committee of the Japan Thyroid Association and Japan Endocrine Society for the establishment of diagnostic criteria and nationwide surveys for thyroid storm. Clin Endocrinol (Oxf). 2016;84(6):912-918.
doi pubmed - Nai Q, Ansari M, Pak S, Tian Y, Amzad-Hossain M, Zhang Y, Lou Y, et al. Cardiorespiratory failure in thyroid storm: case report and literature review. J Clin Med Res. 2018;10(4):351-357.
doi pubmed - Akamizu T. Thyroid Storm: A Japanese Perspective. Thyroid. 2018;28(1):32-40.
doi pubmed - Satoh T, Isozaki O, Suzuki A, Wakino S, Iburi T, Tsuboi K, Kanamoto N, et al. 2016 Guidelines for the management of thyroid storm from The Japan Thyroid Association and Japan Endocrine Society (First edition). Endocr J. 2016;63(12):1025-1064.
doi pubmed - Yanai H, Hakoshima M, Katsuyama H. Differences in clinical and laboratory findings among Graves' disease, painless thyroiditis and subacute thyroiditis patients with hyperthyroidism. J Endocrinol Metab. 2019;9(3):37-42.
doi
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
