| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Case Report
Volume 6, Number 1, February 2016, pages 27-29
A Large Superior Mediastinal Mass: “Terrible Thyroid Cancer”
Shivanand Naveena, Shubhra Chauhana, Nisheena Raghavanb, Naveen Hedne Chandrashekhara, S. V. Srikrishnac, Sanjay Basaveshwara Dhadedd, Subramanian Kannane, f
aDepartment of Head and Neck Surgical Oncology, Narayana Health City, Bangalore, Karnataka, India
bDepartment of Pathology, Narayana Health City, Bangalore, Karnataka, India
cDepartment of Thoracic Surgery, Narayana Health City, Bangalore, Karnataka, India
dDepartment of Cardiac Surgery, Narayana Health City, Bangalore, Karnataka, India
eDepartment of Endocrinology, Diabetes and Bariatric Medicine, Narayana Health City, Bangalore, Karnataka, India
fCorresponding Author: Subramanian Kannan, Department of Endocrinology, Diabetes and Bariatric Medicine, Narayana Health City, 258/A, Bommasandra Industrial Area, Hosur Road, Bangalore, Karnataka 560099, India
Manuscript accepted for publication January 07, 2016
Short title: Superior Mediastinal Mass
doi: http://dx.doi.org/10.14740/jem325w
| Abstract | ▴Top |
Anterior mediastinal masses arise from a diverse group of conditions including thymoma, teratoma, retrosternal goiter, thoracic aortic lesions and lymphoma. We report a case of a 70-year-old male with anterior mediastinal mass who on further evaluation was found to have a large mediastinal lymph node secondary to a papillary thyroid cancer. Metastatic lymph node mass from thyroid malignancy should also be considered as one of the differential diagnosis in the evaluation of anterior mediastinal mass.
Keywords: Thyroid cancer; Mediastinal lymph node; Anterior mediastinal mass
| Introduction | ▴Top |
Evaluation of mediastinal mass is a clinical challenge. Most commonly encountered pathologies include thymoma, thyroid neoplasm, teratoma, thoracic aortic aneurysms and “terrible” aggressive lymphoma [1]. Incidence of ectopic mediastinal goiter accounts for about 1% of all goiters [2]. Retrosternal extension of large goiter into mediastinum is seen in about 7% of all goiters [3], where the extended lobe/nodule is in continuity with the thyroid gland. In rare situation, superior mediastinal lymph nodes could be the result of metastatic lymph nodal deposit from differentiated thyroid malignancy which accounts for about 5% [4]. Here we report a case of an anterior mediastinal mass, which on evaluation turned out to be metastatic lymph node deposit from papillary carcinoma thyroid.
| Case Report | ▴Top |
A 70-year-old man presented to the cardiologist with chest pain and breathlessness on exertion. ECG showed ST-T changes and the chest X-ray surprisingly showed a large antero-superior mediastinal mass (Fig. 1). He was further evaluated with a PET-CT which showed a large cystic mass in the anterior mediastinum measuring 8.4 × 17.4 × 10.9 cm with FDG-avidity in the peripheral wall of the cyst (Fig. 2). FDG uptake was also seen in left lobe of the thyroid (measuring 3 × 3 cm) and in left level IV node (1 × 1 cm) (Fig. 2). Diagnostic coronary angiogram revealed triple vessel disease needing coronary artery bypass grafting. Fine-needle aspiration cytology from the thyroid gland and cervical lymph node was consistent with papillary thyroid carcinoma (PTC).
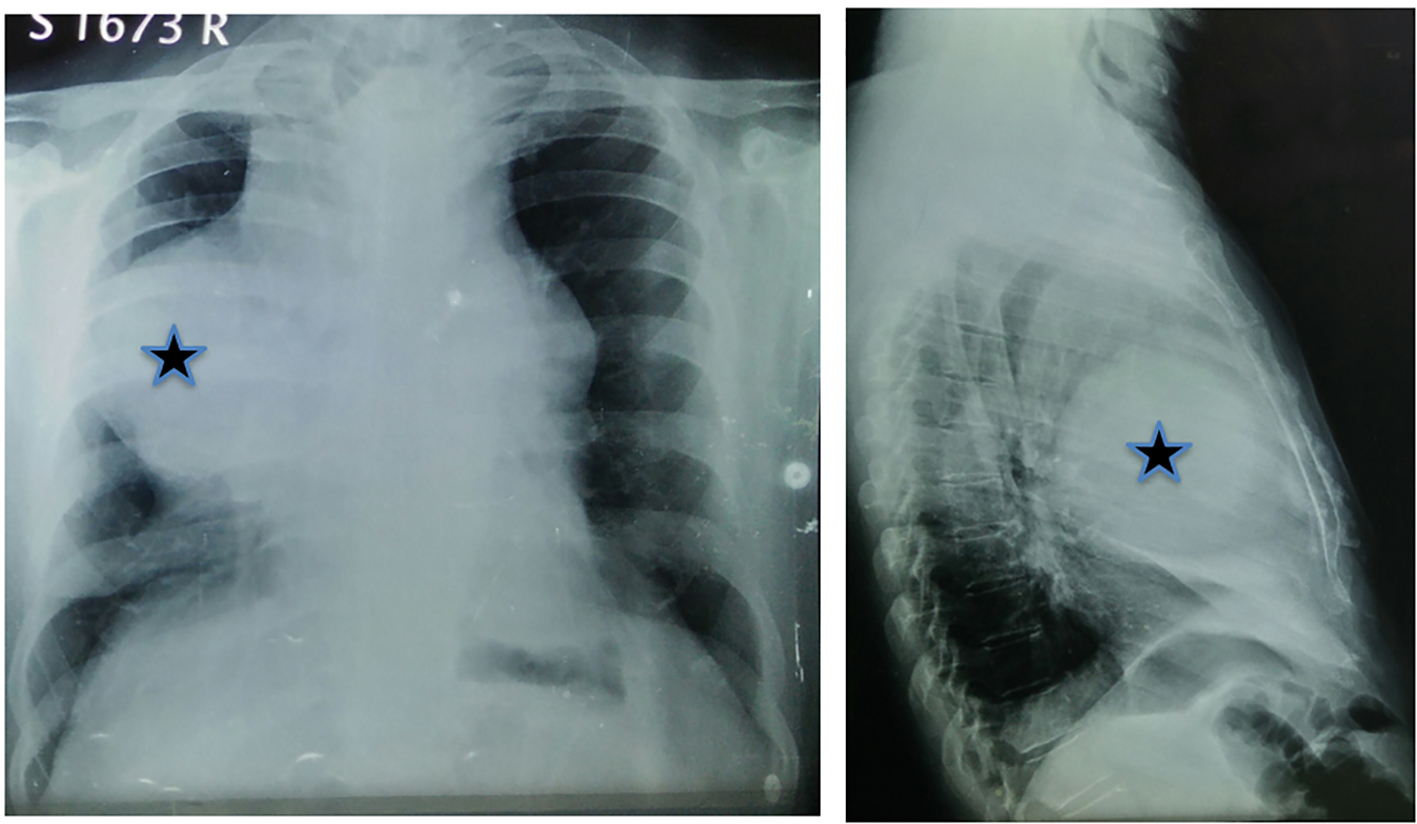 Click for large image | Figure 1. Chest X-ray showing large antero-superior mediastinal mass (star). |
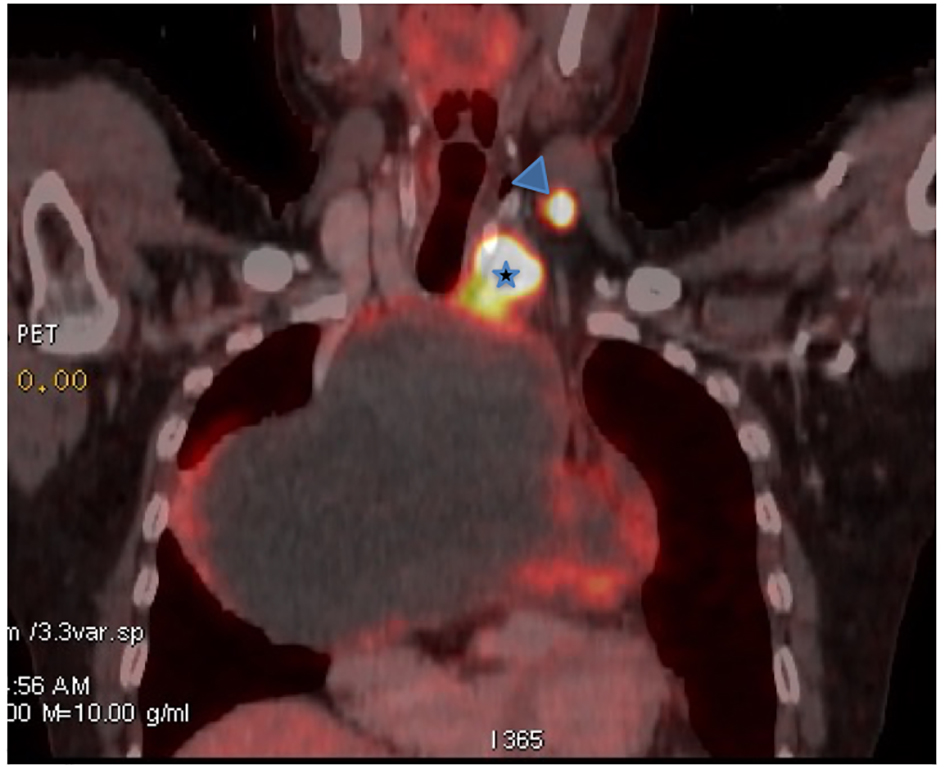 Click for large image | Figure 2. Coronal view FDG-PET-CT: large mediastinal cystic mass with FDG uptake is seen in the periphery of the mass. Also seen is intense FDG uptake on the left lobe thyroid nodule (star) and left level IV cervical lymph node (arrow head). |
Total thyroidectomy was initially done along with central and left lateral compartment neck dissection. Sternotomy was then performed to remove the mediastinal mass en bloc without rupturing the cystic wall followed by coronary bypass surgery. The final histopathology of the thyroid confirmed the diagnosis of PTC (tall cell variant) with metastatic deposits to the cervical nodes. The large mass in the mediastinum was a metastatic lymph node with cystic transformation (Fig. 3). Patient recuperated well and subsequently underwent radio-iodine ablation and is currently on follow-up.
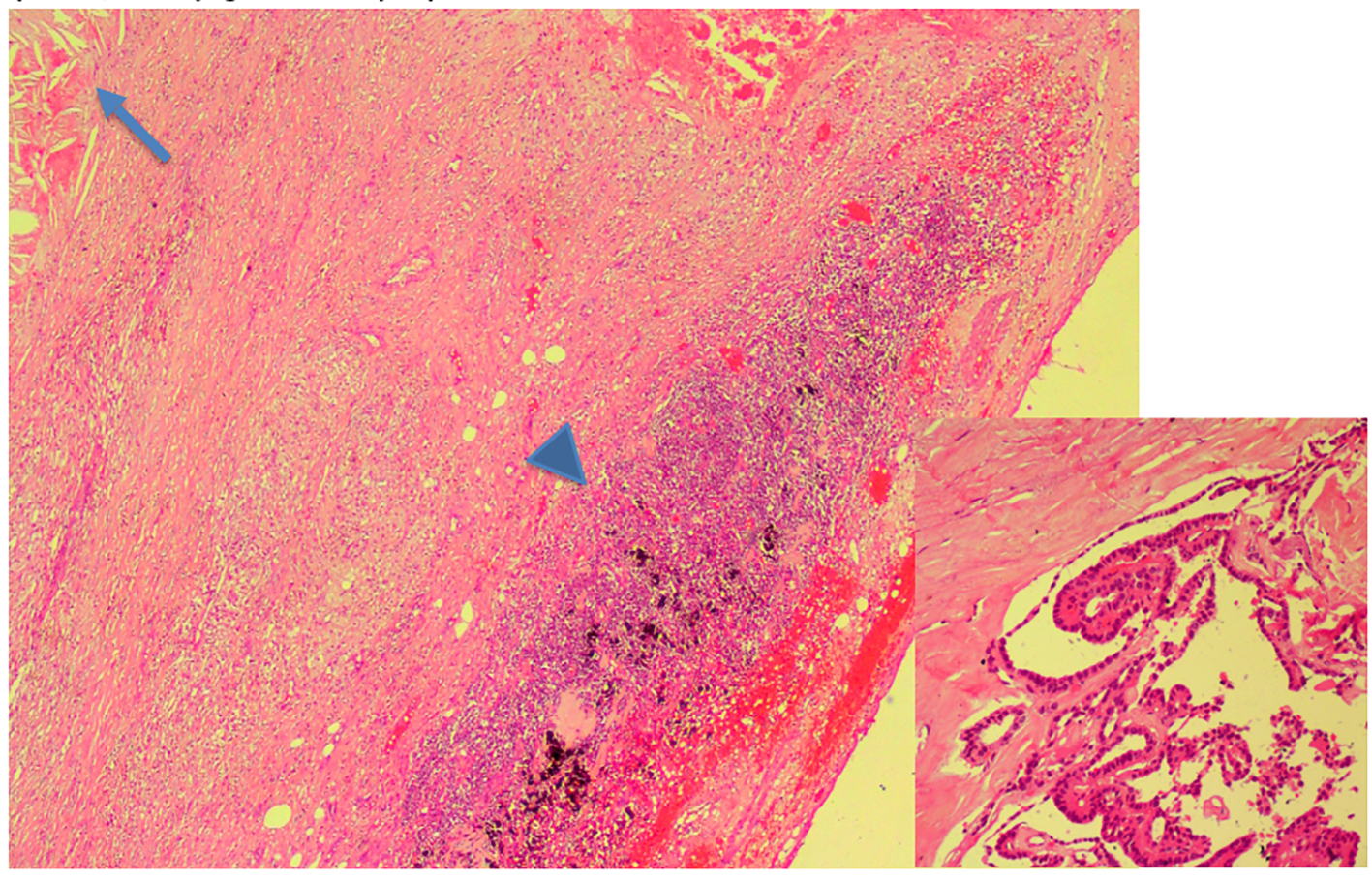 Click for large image | Figure 3. Histopathology (HPE) of mediastinal mass showing cyst wall containing hemorrhage and cholesterol clefts (arrow) with periphery showing the lymphoid follicles with black anthracotic pigment (arrow head). The inset (× 20) shows a focus of long papillae lined by single layer of tall columnar cells with sharply delineated cell borders, intensely eosinophilic, finely granular cytoplasm consistent with tall cell variant of PTC. |
| Discussion | ▴Top |
The differentials of an antero-superior mediastinal mass typically include the five “Ts”, thymoma, thyroid neoplasm, teratoma, thoracic aortic aneurysms and “terrible” lymphoma [1]. Majority of anterior mediastinal masses originating from thyroid are mediastinal goiter representing direct contiguous growth of goiter into the superior mediastinum. However, a large cystic mediastinal mass as a result of lymph node metastasis from a PTC is rather unusual and hence our sixth “T” in the differential of superior mediastinal mass is “terrible thyroid cancer”. Less than 5% of PTCs present with level VII mediastinal lymph nodes [4]. Possible mechanisms of developing mediastinal nodes are two ways either through communication from the under surface of the gland and the other being lymphatics along recurrent laryngeal nerve [5]. Presence of lateral cervical lymph node metastasis and aggressive histological variants is more likely to have mediastinal lymph node involvement [4]. Patients with poor differentiation and suspected distant metastasis should undergo mediastinal imaging [4]. A meta-analysis of nine studies showed no relation between lymph node status at presentation and survival [5]. Surgery remains the mainstay of treatment followed by iodine therapy if curative intent is planned [6]. Addressing anterior mediastinal nodes could be through the same thyroidectomy incision or separately through sternotomy [6]. In our case, we addressed level VII node through sternotomy due to large size of the mass, also needed for the cardiac bypass surgery which was done at the same time. Untreated metastatic mediastinal node from PTC could lead to life-threatening situations by invasion of the disease into surrounding trachea, manubrium and great vessels and pave way for hematogenous spread of tumor [6]. Reports suggest increased risk of damaging recurrent laryngeal nerve, hypoparathyroidism, chyle leak, and injury to mediastinal vessels while addressing level VII group of nodes [7]. Careful maneuvering would cause least amount of morbidity. In the present day with increased use of ultrasonography and FNAC, ability to diagnose thyroid malignancies at early stages and appropriate management is possible, hence decreasing the incidence of mediastinal lymphadenopathy [6].
Conclusion
Nodal metastasis from thyroid malignancies should be considered as the sixth “T” during the evaluation of an anterior mediastinal mass.
Author Contributions
All authors were involved in the clinical care of the patient. Authors SK, NBS, and NR were involved in the preparation of the manuscript.
Conflicts of Interest
None.
Funding Source
None.
| References | ▴Top |
- Juanpere S, Canete N, Ortuno P, Martinez S, Sanchez G, Bernado L. A diagnostic approach to the mediastinal masses. Insights into Imaging. 2013;4(1):29-52.
doi pubmed - Clark G, Russell J, Dudley B, Christie III, William M T, Martin D. Ann thoracic surg. 2003:1952-1953.
- Newman E, Saha A R. Substernal goiter. Journal of Surgical Oncology. 1995;60(3):207-212.
doi pubmed - Machens A, Dralle H. Prediction of mediastinal lymph node metastasis in papillary thyroid cancer. Ann Surg Oncol. 2009;16(1):171-176.
doi pubmed - Grebe SK, Hay ID. Thyroid cancer nodal metastases: biologic significance and thera-peutic considerations. Surg Oncol Clin N Am. 1996;5(1):43-63.
pubmed - Melvin A B, Martin M, Robert H. Significance of mediastinal lymphnodes from car-cinoma of thyroid. American Journal of Surgery. 1972;123:702-705.
doi - White ML, Gauger PG, Doherty GM. Central lymph node dissection in differentiated thyroid cancer. World J Surg. 2007;31(5):895-904.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
