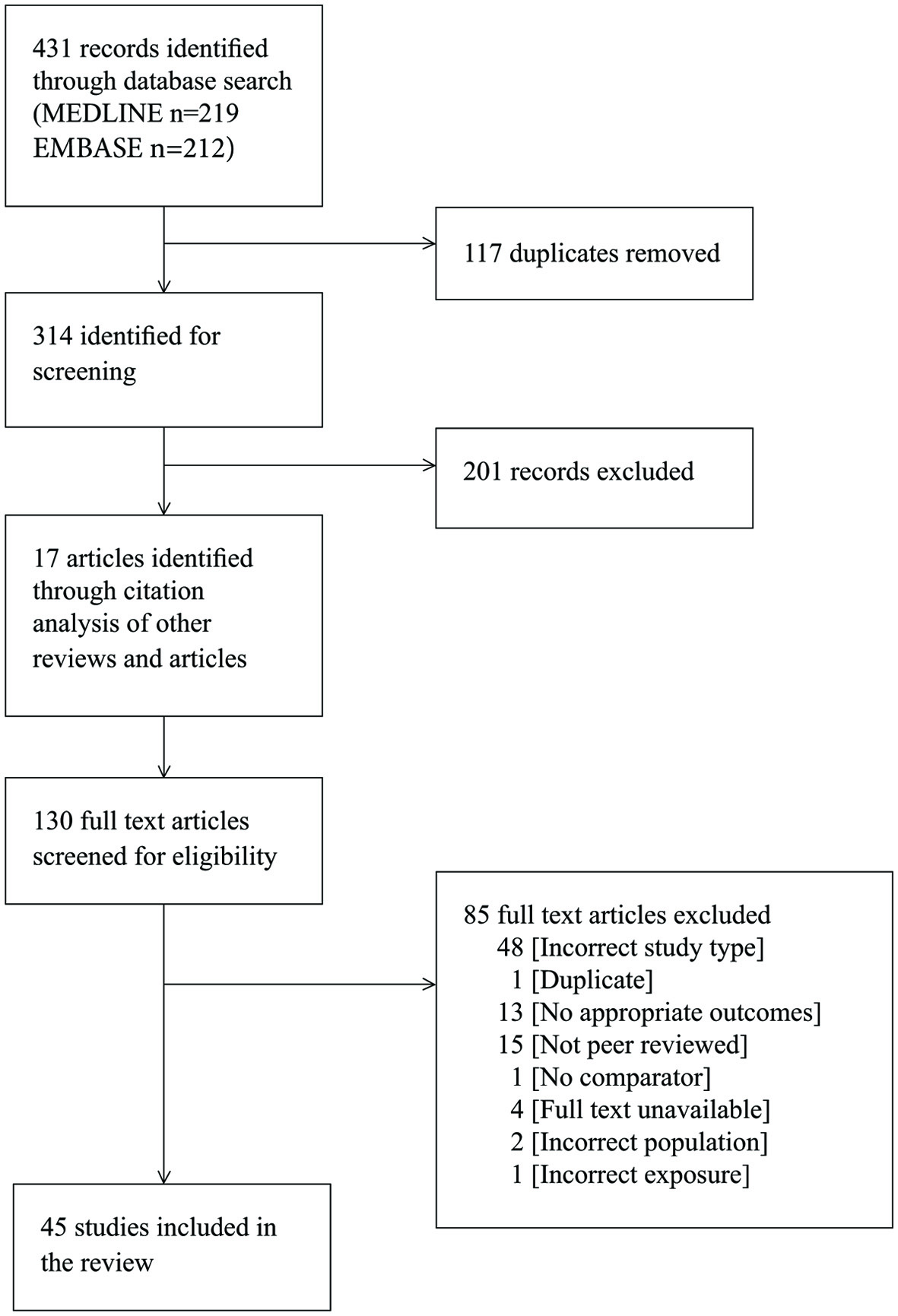
Figure 1. PRISMA flow diagram showing results of search and study selection.
| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Original Article
Volume 10, Number 5, October 2020, pages 118-130
Association of Diabetes and Severe COVID-19 Outcomes: A Rapid Review and Meta-Analysis
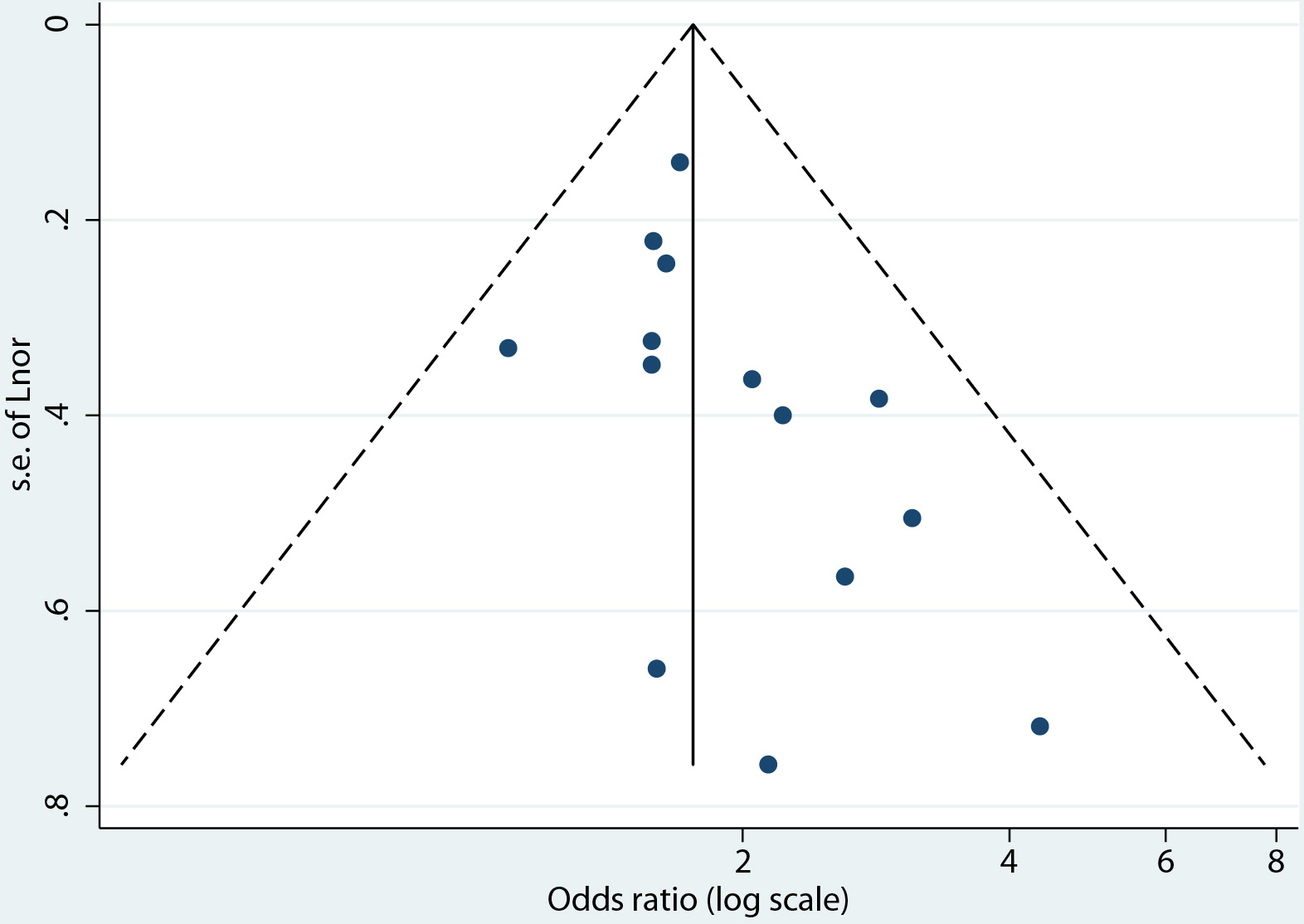
Figures
Tables
| Total patients analyzed | Setting | Timeframe | Exposure | Outcome | Adjustment | |
|---|---|---|---|---|---|---|
| Guan WJ et al, 2020 [29] | 1,590 | 575 hospitals in 31 provinces/autonomous regions/provincial municipalities across mainland China | December 11, 2019 to January 31, 2020 | Self-report | Composite endpoint (admission to ICU, IMV, or mortality) vs. no composite endpoint | Age and smoking status |
| Hu L et al, 2020 [33] | 323 | Tianyou Hospital, Wuhan, Hubei Province, China | January 8 to February 20, 2020 with follow-up until March 10, 2020 | Medical history | Progressive disease vs. non-progressive disease of patients classified as non-severe, severe, and critical at baseline | None |
| Huang R et al, 2020 [2] | 202 | 8 designated hospitals in 8 cities of Jiangsu Province, China | January 22 to February 10, 2020 | Medical history | Severe vsx non-severe disease | Obesity (BMI > 28), lactate dehydrogenase (LDH) > 250 U/L, ALB < 35 g/L, and CRP > 10 mg/L |
| Hur K et al, 2020 [35] | 486 | 10 hospitals in the Chicago metropolitan area, Illinois, USA | March 1 to April 8, 2020 with follow-up until April 18 2020 | Medical history | IMV or discharge from hospital | Selected variables of importance from the random forest model |
| Mo P et al, 2020 [38] | 155 | Zhongnan Hospital of Wuhan University, Wuhan, Hubei Province, China | January 1 to February 5, 2020 | Medical records | Refractory disease (not responding to treatment) vs. non-refractory disease | Variables identified by univariate analysis |
| Shi Q et al, 2020 [40] | 306 | Renmin Hospital of Wuhan University and Zhongnan Hospital of Wuhan University, Wuhan, Hubei Province, China | January 1 to March 8, 2020 | Medical records | Mortality vs. discharged from hospital | Hypertension, cardiovascular disease, chronic pulmonary disease |
| Simonnet A et al, 2020 [41] | 124 | CHRU Lille, Nord - Pas de Calais, France | February 27 to April 5, 2020 | Medical records | IMV vs. non-IMV | Age, sex, hypertension, dyslipidaemia, BMI |
| Targher G et al, 2020 [42] | 339 | 4 unnamed sites in Zhejiang Province, China | January and February, 2020 | Self-reported or random plasma glucose or HbA1c | Severe and critical disease vs. mild and moderate disease | Age, sex, obesity, hypertension, smoking |
| Wang L et al, 2020 [46] | 339 | Renmin Hospital of Wuhan University, Wuhan, Hubei Province, China | January 1 to February 6, 2020 with follow-up until March 5, 2020 | Medical history | Mortality vs. discharged from hospital | Comorbidities, complications, age |
| Wu C et al, 2020 [50] | 201 | Jinyintan Hospital, Wuhan, Hubei Province, China | December 25, 2019 to January 26, 2020 | Medical records | Mortality vs. discharged from hospital | Not reported |
| Zhang X et al, 2020 [58] | 645 | Various designated hospitals according to the government emergency rule of Zhejiang Province, Zhejiang, China | January 17, to February 8, 2020 | No description | Severe vs. non-severe disease | Not reported |
| Zhang Y et al, 2020 [59] | 145 | Tongji Hospital, Wuhan, Hubei Province, China | February 8 to March 21, 2020 | Medical history | Composite endpoint (admission to ICU, IMV, or mortality) vs. no composite endpoint | Age, sex, BMI, medical histories of hypertension, cardiovascular disease, and malignancy |
| Zhou F et al, 2020 [61] | 191 | Jinyintan Hospital and Wuhan Pulmonary Hospital, Wuhan, Hubei Province, China | 29 December 2019 - 31 January 2020 | Medical records | Mortality vs. discharged from hospital | None |
| Zhu L et al, 2020 [62] | 7,337 | 19 hospitals, Hubei Province, China | 30 December 2019 - 20 March 2020 | Medical history or clinical diagnosis | Mortality vs. discharged from hospital | Age, gender, hospital site on admission, with no adjustment for comorbidities closely related to type 2 diabetes (hypertension, CHD, cerebrovascular disease, and chronic kidney disease) |
| Uncontrolled hyperglycemia | A retrospective cohort study (n = 570) in the USA investigating blood glucose levels among hospitalized patients with diabetes for acute hyperglycemia found that there is an association. The study reported that hospitalized COVID-19 patients with diabetes and/or uncontrolled hyperglycemia had a higher prevalence of mortality as compared with patients without diabetes or uncontrolled hyperglycaemia [20]. Diabetes was defined as A1c ≥ 6.5% [20]. Uncontrolled hyperglycemia was defined as ≥ 2 blood glucoses (BGs) > 180 mg/dL within any 24-h period [20]. However, the CORONADO prospective cohort study with 1,317 COVID-19 patients with diabetes from 53 hospitals in France, where the HbA1C level of the patients was examined, did not find that long-term glycemic control impacted the severity of COVID-19 disease within the first 7 days of admission to hospital [5]. |
| Insulin use | A retrospective study of patients with diabetes (n = 136) and those without diabetes (n = 768) with moderate, severe, or critical COVID-19 in Wuhan, China, noted the use of insulin in patients with diabetes was related to poor prognosis of COVID-19 clinical course [25]. However, in the CORONADO study, insulin use was not associated with a severe prognosis (intubation and/or death on day 7) in a multivariable analysis after adjustment [5]. Insulin use may be a proxy of advanced diabetes in older people with complications such as chronic kidney disease (CKD), rather than a causal factor of COVID-19 severity [5]. |
| Triglyceride and glucose (TyG) index marker for insulin resistance | A retrospective study of 151 patients in Wuhan, China, who were admitted to hospital with moderate to severe COVID-19 found an increasing TyG index to predict increased odds of severe or mortal outcomes from COVID-19 [39]. |