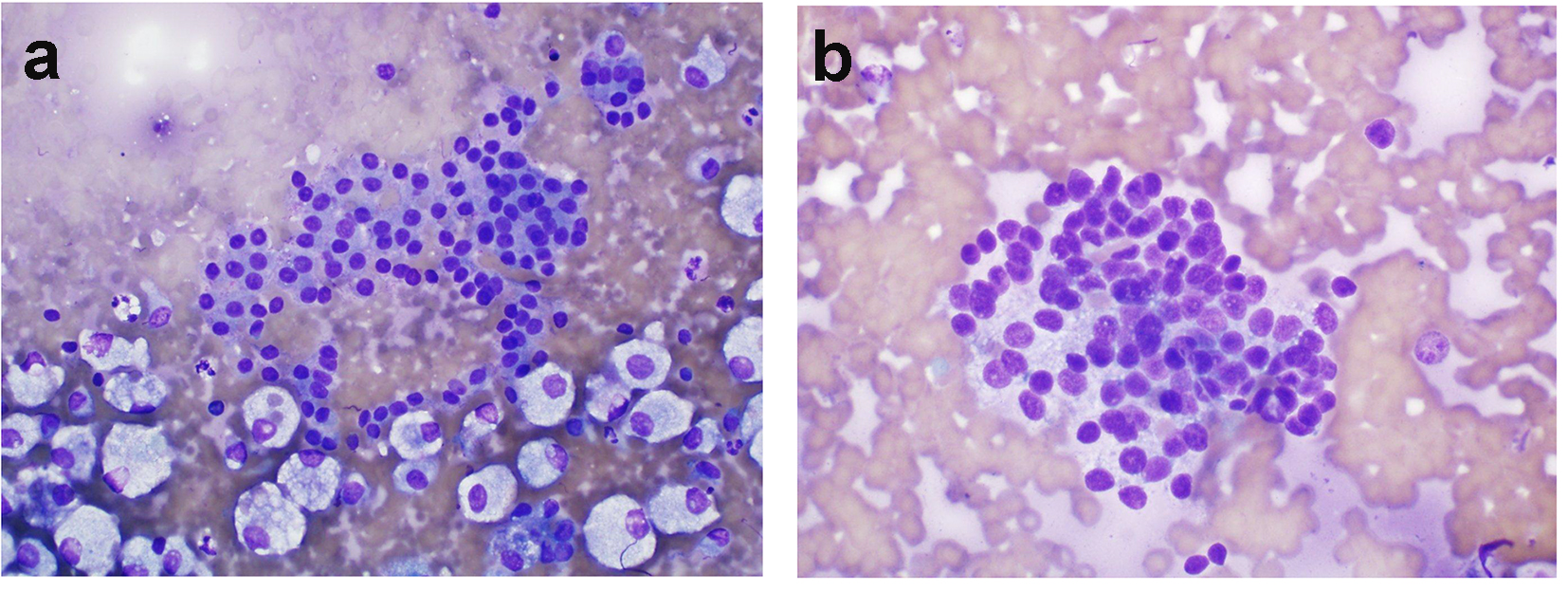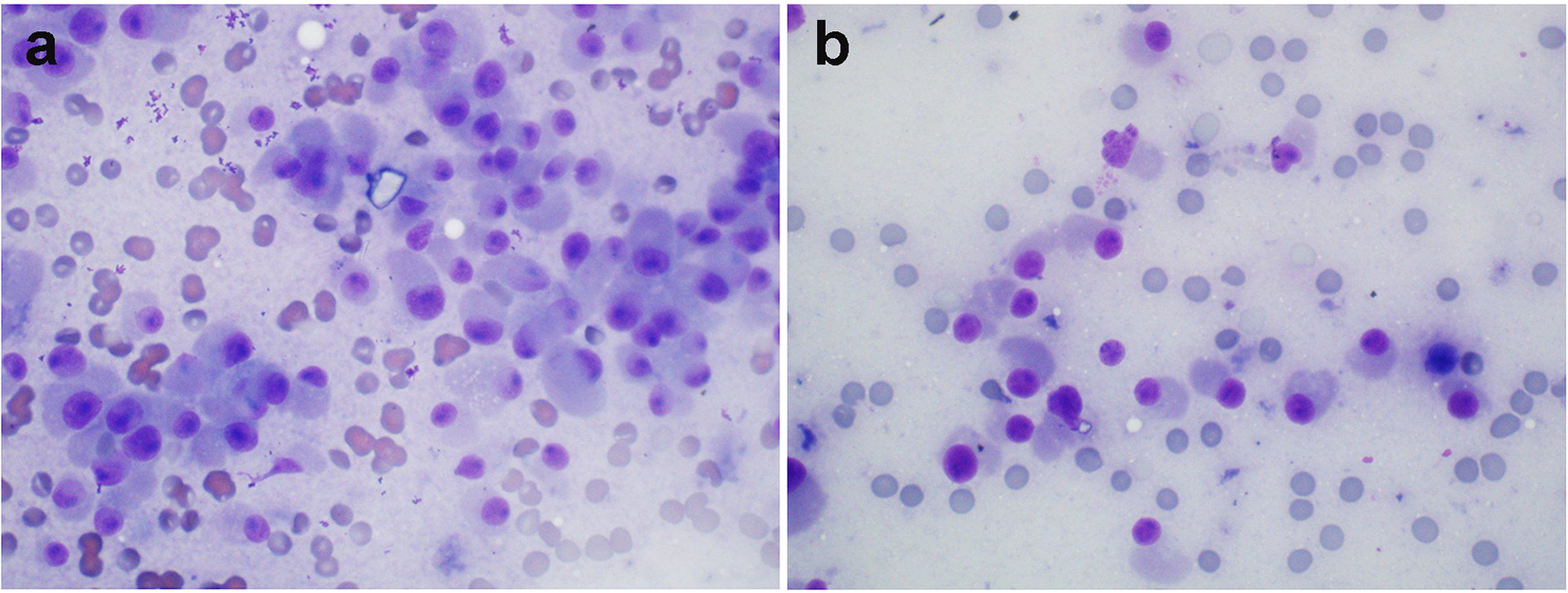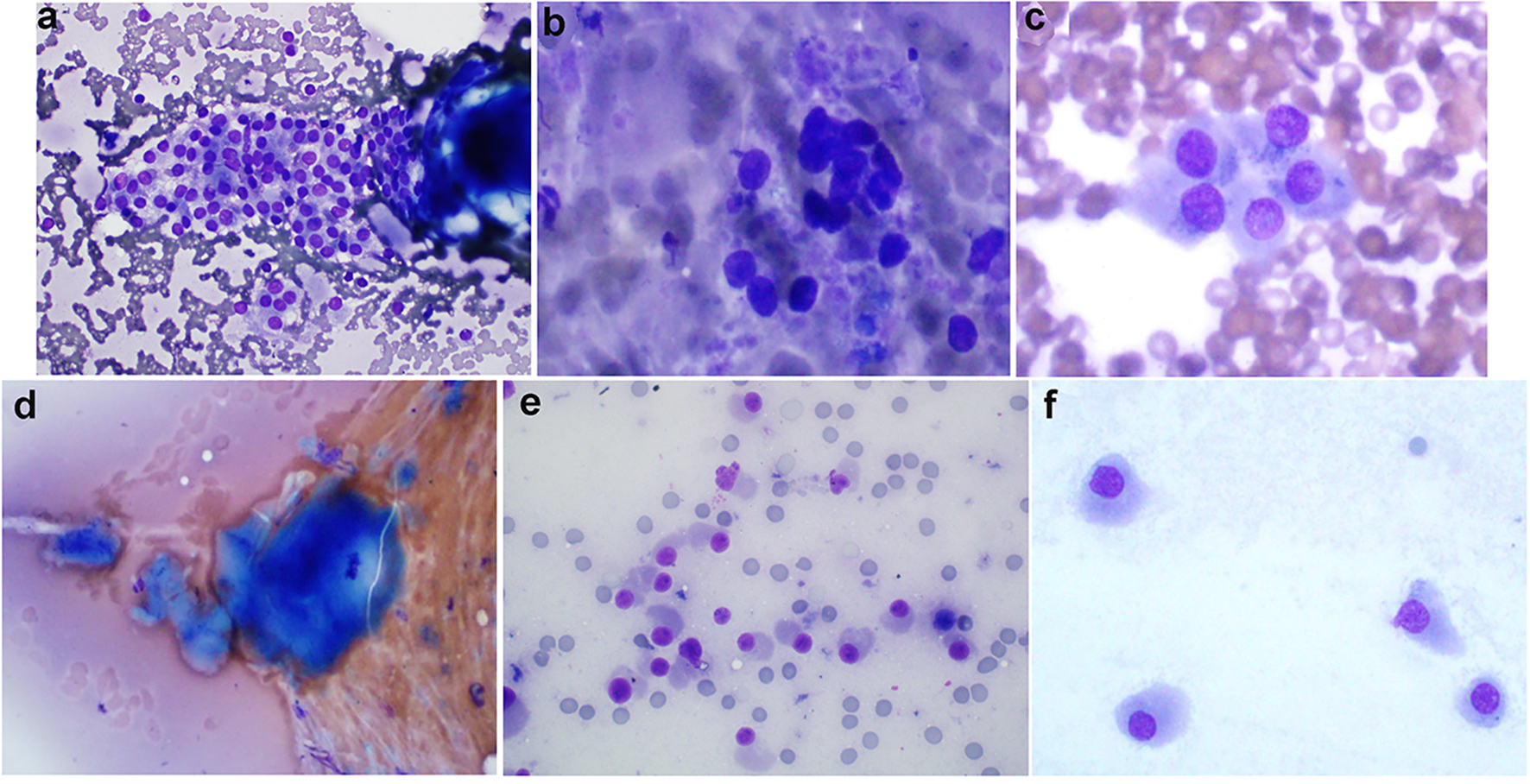
Figure 1. (Patient 1) (a) Results of FNB biopsy of the right thyroid nodules (two nodules, 1a and 1b biopsied together): follicular cells trying to form microfollicles. Follicular cells show some degree of atypia. These features suggest follicular lesions of undetermined significance (Diff-Quik, × 600). (b) Results of FNB biopsy of the left thyroid nodule (nodule 2a): follicular cells forming microfollicles. Follicular cells show some degree of atypia. These features suggest follicular lesions of undetermined significance (Diff-Quik, × 600). (c) Results of MFNB biopsy of the right thyroid nodules (two nodules, 1a and 1b biopsied together): cellular smears consisting of discohesive cells with abundant amphophillic cytoplasm, and eccentrically placed nuclei with prominent nucleoli. These features along with elevated serum calcitonin suggest medullary thyroid cancer (Diff-Quik, × 600). (d) MFNB of the left thyroid nodule (nodule 2a): amorphous material suggestive of amyloid material (Congo red stain not done) (Diff-Quik, × 600). (e) MFNB of the left thyroid nodule (nodule 2a): crowded groups of mildly enlarged cells with oval to focally spindled nuclei, moderate to abundant cytoplasm and finely stippled chromatin. While not classic for medullary carcinoma, the concurrent finding of elevated serum calcitonin makes the diagnosis more likely (Diff-Quik, × 600). (f) MFNB of the left thyroid nodule (nodule 2a): cells with oval to focally spindled nuclei, abundant cytoplasm and finely stippled chromatin. While not classic for medullary carcinoma, the concurrent finding of elevated serum calcitonin makes the diagnosis more likely (Diff-Quik, × 600). FNB: fine-needle biopsy; MFNB: modified fine-needle biopsy; Diff. quick: Diff quick stain.