| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Original Article
Volume 7, Number 6, December 2017, pages 185-189
Assessment of Diabetes Knowledge Using the Michigan Brief Diabetes Knowledge Test Among Patients With Type 2 Diabetes Mellitus
Turki M. Almalkia, Naif R. Almalkia, Khalid Balbaidb, Khaled Alswata, c
aTaif University School of Medicine, Taif, Saudi Arabia
bKing Abdulaziz Specialist Hospital, Taif, Saudi Arabia
cCorresponding Author: Khaled A. Alswat, Taif University School of Medicine, Taif, Saudi Arabia
Manuscript submitted November 20, 2017, accepted December 5, 2017
Short title: Michigan Brief Diabetes Knowledge Test
doi: https://doi.org/10.14740/jem473w
| Abstract | ▴Top |
Background: Type 2 diabetes mellitus (T2DM) represents a growing health threat globally. The International Diabetes Federation (IDF) estimated that 387 million adults had diabetes in 2014, and this number is expected to continue to grow. In Saudi Arabia, the prevalence of T2DM over time has increased. Diabetes knowledge has been shown to improve self-management skills and glycemic control. The primary goal of this study was to assess diabetes knowledge and its impact on diabetes control and complications.
Methods: We conducted a cross-sectional study at King Abdulaziz Specialist Hospital, Taif City, Saudi Arabia, Division of Endocrinology. T2DM patients older than 18 years who underwent a routine visit to the endocrine clinic between June and October 2014 were asked to participate. Baseline characteristics and measurement were obtained at the time of visit. Laboratory data were collected from the patients’ medical records. We excluded patients with type 1 diabetes mellitus (T1DM). We used the Michigan Brief Diabetes Knowledge Test to assess patients’ knowledge. Those patients who answered ≥ 65% of the questions were considered to possess good knowledge about diabetes.
Results: A total of 264 patients participated; 131 (49.6%) were male and 132 (50.0%) were female. Approximately, half of the patients (44.7%) had had diabetes for at least 10 years, and 29.8% of patients had had the disease for 5 - 10 years. The cohort’s mean A1c was 8.56% and mean body mass index was 30.5%. Sixty-four percent of patients had only a high school education or less, and 38% had at least a college degree. Approximately, half of the cohort (41.7%) were considered to be low income, 37.9% were on oral medications only, and 41.3% were on insulin. The mean fraction of correctly answered knowledge questions was 48.26%. Twenty-eight percent of the participants thought that A1c reflected blood glucose control over the past week, and 44.3% did not know what A1c was. Approximately, one-third of patients (29.5%) believed that diet soda could be used to treat low blood glucose. Fifty-seven patients (21.6%) were considered to have good knowledge about diabetes.
Conclusion: The majority (78.4%) of the screened T2DM patients had poor knowledge about diabetes. Poor knowledge was associated with higher A1c, a non-significant increase in the majority of measured cardiovascular markers, and less awareness of diabetes-related complications.
Keywords: Diabetes knowledge; Type 2 diabetes; Awareness; Assessment
| Introduction | ▴Top |
Diabetes is a common disease worldwide. The International Diabetes Federation (IDF) has subsequently released estimates of the numbers of people living with diabetes in 2003 and a forecast of the affected population in 2025 (194 million and 334 million, respectively) [1]. Although the prevalence of diabetes mellitus (DM) is high among populations in the Middle East and Gulf countries, patients often lack the knowledge and skills to self-manage their condition [2]. Almost three decades ago, the population of the Kingdom of Saudi Arabia went huge changes in lifestyle, primarily leading to decreased physical activity and unhealthy eating habits [3]. These changes have had a considerable negative impact on the health of the society. Indeed, this lifestyle transformation is believed to be responsible for the epidemic of non-communicable diseases and their complications in the country [3]. It is thought that effective diabetes education and knowledge can improve self-management skills and glycemic control for patients with type 2 diabetes mellitus (T2DM) [4] and positively affect the health system. However, there is still a lack of studies that have assessed awareness and knowledge among diabetic patients in Saudi Arabic and more specifically in Taif City despite the high prevalence. Cross-sectional studies have suggested that the prevalence of T2DM in Saudi ranges from 10% to 30% [4].
The management of DM largely depends on patients themselves [5]. Therefore, patient education is always an important element of DM management [5]. Diabetes knowledge has been shown to improve self-management skills and glycemic control in patients with T2DM [4]. Several recent studies conducted in many parts of the world have suggested that there is a lack of public knowledge about various aspects of diabetes and that an enormous number of patients lack the skills to self-manage their condition [6]. The primary goal of this study was to assess diabetes knowledge and its impact on diabetes control and complications.
| Research Methodology | ▴Top |
A cross-sectional study was conducted between June 2014 and October 2014 at King Abdulaziz Specialized Hospital (KASH), Division of Endocrinology Taif City, Saudi Arabia. Random sampling was used to ensure that the participants were representative of the whole population. The study included 264 patients with T2DM older than 18 and who were willing to participate. We excluded patients with type 1 diabetes mellitus (T1DM) and patients with gestational diabetes. Data were collected through a formal interview with the patients conducted by one of the researchers. Baseline characteristics and measurements such as blood pressure, height and body weight were obtained at the time of visit. Laboratory data were collected from each patient’s electronic medical record (EMR). This cross-sectional study used a questionnaire known as the Michigan Brief Diabetes Knowledge Test to assess each patient’s knowledge [7-10].
This questionnaire was also translated into Arabic. The Arabic version of the questionnaire was used to reduce language barriers among patients. The questionnaire consisted of 20 true/false statements that aimed to assess DM knowledge and awareness. Patients who answered > 65% of the questions correctly were considered to possess good knowledge about DM. Socioeconomic data such as smoking, physical exercise, T2DM duration and education level were self-reported. All of the data were collected and analyzed using the statistical software SPSS version 20.0 (IBM, Chicago). We used frequency for category variables and mean and standard deviation (SD) for continuous variables. The Chi-squared test was used to study the relation between variables; we used the t-test to compare means. P value less than 0.05 is statistically significant.
| Results | ▴Top |
A total of 264 patients participated, 131 (49.6%) males and 132 (50.0%) females. The mean age of the cohort was 53.2 years (SD: 13.4 years), and 44.7% of patients had had diabetes for at least 10 years. Approximately, one-third of patients (29.8%) had had the disease for 5 - 10 years. The mean A1c was 8.6%, the mean body mass index (BMI) was 30.5%, 66% of patients were married, 64% possessed a high school or lower level of education, 38% possessed at least a college degree, 41.7% were considered to be low income, 38% were on oral medications only, 41.4% were on insulin, 20.5% were on insulin ± oral, and the mean fraction of correctly answered knowledge questions was 48.3%. Approximately, one-third of the cohort (28%) believed that A1c reflected blood glucose (BG) control over the past week and 44.3% of patients did not know what A1c was (Fig. 1). Approximately one in three patients believed that diet soda could be used to treat low BG, 34.8% did not know and 35.6% did not think so (Fig. 2).
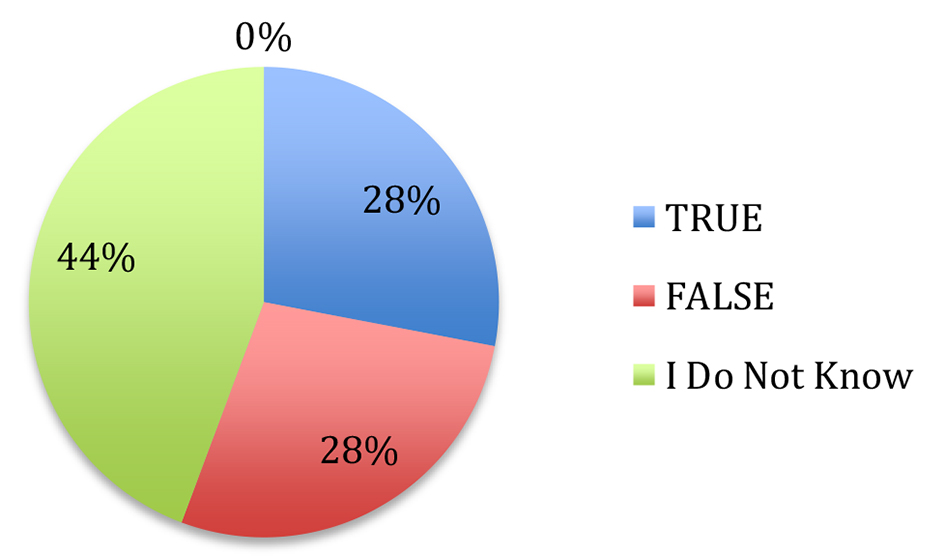 Click for large image | Figure 1. HbA1c is a test that measures your average blood glucose level in the past week. |
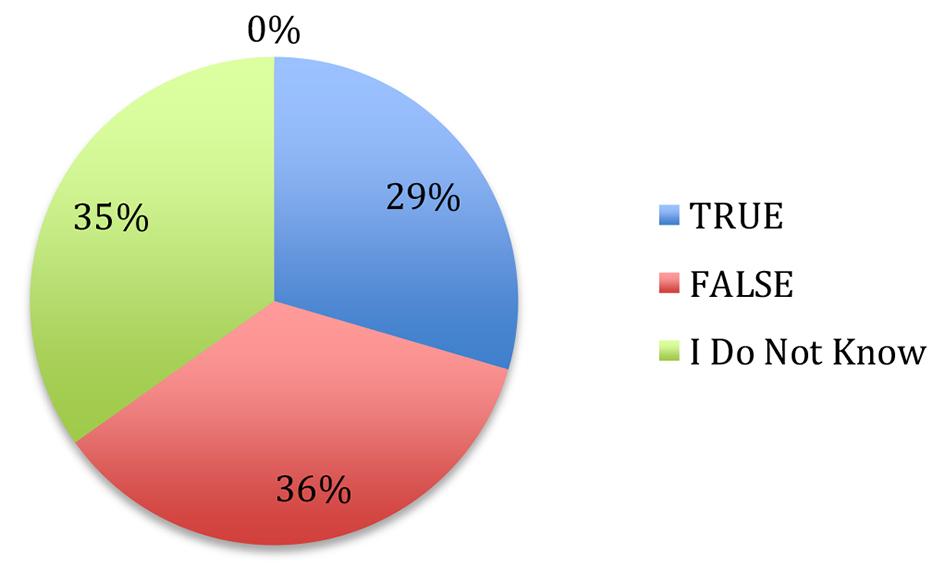 Click for large image | Figure 2. A can of diet soft drink can be used for treating low blood glucose levels. |
Fifty-seven patients (21.6%) were considered to possess good knowledge about diabetes. Compared with those with poor knowledge, diabetics with good knowledge of their disease had a mean age of 49 years vs. 54 years (P < 0.05), 56.1% were male vs. 44% female (P = 0.28), and 59.7% vs. 28.5% had a college degree or higher (< 0.05). Of diabetics, 76.4% with good knowledge reported a sedentary lifestyle compared with 85.5% who had poor knowledge (P = 0.10). Approximately, 14.5% of the diabetics with good knowledge were active smokers compared with 13.5% of patients with poor knowledge (P = 0.83). Diabetics with good knowledge had a mean A1c of 7.6 vs. 8.8 (P < 0.05), a mean BMI of 30.6 vs. 30.5, a mean systolic blood pressure (SBP) of 136.5 vs. 148.4 (P = 0.01), a mean resting heart rate of 73.1 vs. 73.8 (P = 0.70), a mean total cholesterol (TC) of 167.2 vs. 176.3 (P < 0.05), a mean LDL of 108.6 vs. 143.10 (P < 0.05), a mean HDL of 44 vs. 41 (P = 0.20), and a mean triglycerides (TG) of 167.4 vs. 183.6 (P = 0.11). Table 1 and Table 2 show baseline characteristics of whole study.
 Click to view | Table 1. Baseline Characteristics of the Entire Cohort |
 Click to view | Table 2. Baseline Characteristics of the Entire Cohort |
All of the diabetics with good knowledge were aware that poorly controlled diabetes causes retinopathy compared with 74% of diabetes with poor knowledge (P < 0.05) (Fig. 3).
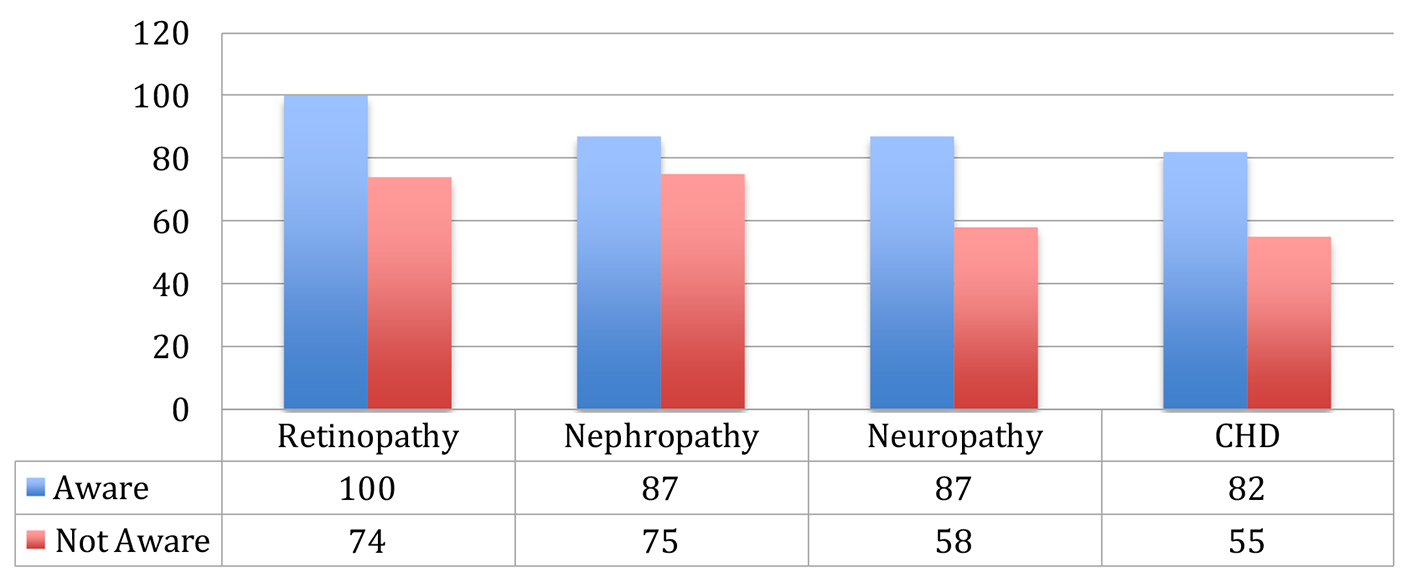 Click for large image | Figure 3. Complication awareness (%). |
The corresponding data for coronary heart disease (CHD) and nephropathy were 82.5% vs. 55.2% (P < 0.05) and 87.7% vs. 75.7% (P = 0.13), respectively.
| Discussion | ▴Top |
The majority of studies have reported that diabetes knowledge and awareness is generally poor between T2DM patients [6-8]. However, it is difficult to compare our results with those of other studies that used different instruments to assess knowledge among diabetic patients. Our study revealed that the level of awareness and knowledge was low among diabetic patients. For example, 28% of the patients thought that A1c reflected BG control over the past week and 44.3% did not know what A1c was. Approximately, one-third of patients (29.5%) thought that diet soda could be used to treat low BG, 34.8% did not know and 35.6% did not think so. We noted that most of the patients who were low income and had low education levels also had low awareness about diabetes complications. Therefore, these patients must be taught about their condition. Patients who have had T2DM for more than 10 years were less aware than those who have had T2DM for 5 - 10 years. Younger diabetic patients are more aware of their condition than elderly diabetic patients, but even patients who are aware of their diabetes report sedentary lifestyle, which gives us a clue that there is a gap between awareness and practice.
We found a correlation between high glycemic control and low level of knowledge among screened T2DM patients. However, some other studies have reported no correlation between these factors [9]. We believe that it is essential to direct more resources to improve knowledge because it has a very effective impact on improving patient compliance and self-care. Since our study was outpatient hospital-based, we faced some limitations such as patients being unwilling to complete the questionnaire and incomplete laboratory findings in some patients’ files.
Conclusion
The majority (78.4%) of the screened T2DM patients were considered to have poor knowledge about diabetes. Poor knowledge was associated with higher A1c, a non-significant increase in the majority of measured cardiovascular markers, and less awareness about diabetes-related complications.
Conflict of Interest
None.
Funding
None.
| References | ▴Top |
- Atlas D. Brussels. International Diabetes Federation. 2003.
- Al-Adsani AM, Moussa MA, Al-Jasem LI, Abdella NA, Al-Hamad NM. The level and determinants of diabetes knowledge in Kuwaiti adults with type 2 diabetes. Diabetes Metab. 2009;35(2):121-128.
doi pubmed - Alwan AD. Noncommunicable diseases: a major challenge to public health in the Region. Eastern Mediterranean health journal. 1997;3(1):6-16.
- Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561-587.
doi pubmed - Powell CK, Hill EG, Clancy DE. The relationship between health literacy and diabetes knowledge and readiness to take health actions. Diabetes Educ. 2007;33(1):144-151.
doi pubmed - Al-Khawaldeh OA, Al-Jaradeen N. Diabetes awareness and diabetes risk reduction behaviors among attendance of primary healthcare centers. Diabetes Metab Syndr. 2013;7(3):172-178.
doi pubmed - The Michigan Diabetes Research and Training Center (MDRTC), University Michigan Health System website. Available: http://www.med.umich.edu/ mdrtc/profs/survey.html. (2013, accessed 4 Jun 2012).
- Ben Abdelaziz A, Thabet H, Soltane I, Gaha K, Gaha R, Tlili H, Ghannem H. [Knowledge of patients with type 2 diabetes about their condition in Sousse, Tunisia]. East Mediterr Health J. 2007;13(3):505-514.
pubmed - Khan LA, Khan SA. Level of knowledge and self-care in diabetics in a community hospital in Najran. Ann Saudi Med. 2000;20(3-4):300-301.
doi pubmed - Al-Maskari F, El-Sadig M, Al-Kaabi JM, Afandi B, Nagelkerke N, Yeatts KB. Knowledge, attitude and practices of diabetic patients in the United Arab Emirates. PLoS One. 2013;8(1):e52857.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.









